To Issue 147
Citation: Schneider A, “How Patient and Treatment Factors Shape Subcutaneous Dosing Preferences.” ONdrugDelivery, Issue 147 (May 2023), pp 15–18.
Andreas Schneider highlights the importance of understanding the drivers of dosing preferences when it comes to choosing the right injection device for patients. Specifically, the research summarised here studies whether and how patient characteristics and treatment attributes influence the decision to use prefilled handheld autoinjectors or large-volume wearable injectors.
Advancements in subcutaneous drug delivery have led to a transformation in healthcare, with more patients self-injecting high-value biologics at home instead of receiving intravenous infusions in the hospital. As a result, choosing the optimal dosing option for medication has become a critical issue that can determine treatment adherence and health outcomes.
“The decision on which dosing option to choose can significantly influence a patient’s therapy adherence, treatment outcomes and total healthcare costs.”
Patricia, a 73-year-old patient with high cholesterol, faced a dilemma when discussing the different dosing options for Repatha (evolocumab, Amgen, CA, US) with her cardiologist. Repatha is an injectable biologic drug to lower bad cholesterol and reduce heart attack risk. Patricia was torn between two options: a twice-weekly 15-second at-home self-injection with a handheld autoinjector or a once-a-month five-minute self-injection with a large-volume wearable device. She was worried about the hassle of injecting herself every two weeks – but felt intimidated by a device attached to her skin for a longer duration. When she asked her doctor to help her decide, he said there was no simple answer to her question.
Every patient is unique, and there is no clear guideline to predict which dosing option would work best for her. Some patients prefer the hands-free operation of the wearable large-volume injector, while others prefer the handheld autoinjector’s feel of control and short injection duration.
Pharmaceutical manufacturers of high-value injectable biologics have taken up patient-centred concepts of self-care by offering more treatment choices. As such, the industry is witnessing an ever-increasing interest in wearable large-volume injectors as an alternative to the market-proven device category of handheld prefilled autoinjectors. Patients can patch these devices onto the skin and self-administer larger dose volumes over minutes or hours, without the need to hold the device against the injection site.
This emerging device category enables the administration of larger single-volume doses of biologics across chronic diseases. In so doing, wearable large-volume injectors contribute to decreasing injection frequency – a critical treatment attribute that scholars have repeatedly related to better treatment adherence. Moreover, these devices also allow for subcutaneous injections for therapies that require single large-volume doses beyond the capacity of handheld autoinjectors. Figure 1 contrasts the key attributes and differences between wearable large-volume injectors and handheld autoinjectors.
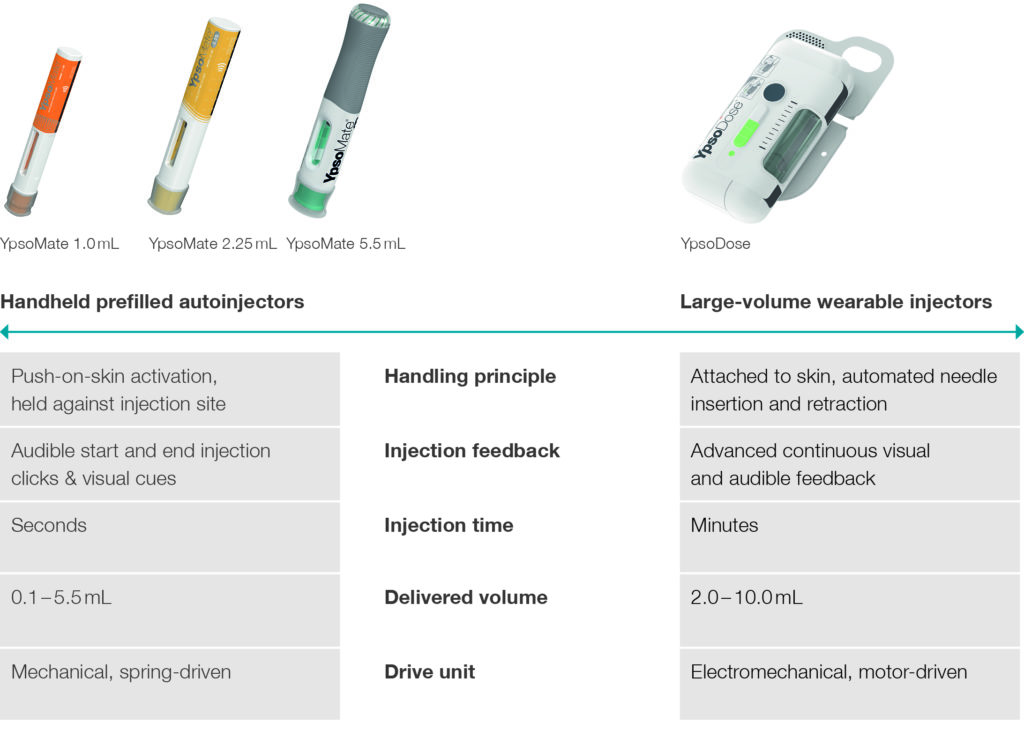
Figure 1: Contrasting prefilled handheld autoinjector with large-volume wearable injector dosing options.
“Patients with multiple sclerosis were most likely to prefer the wearable device, while those with psoriasis were least likely.”
As patients like Patricia are taking a more active role in treatment decisions, healthcare providers are encouraged to personalise therapy options to ensure optimal medication adherence and health outcomes. However, the industry offers few answers to whether and how patient characteristics and therapy attributes drive device choices. This lack of insights is critical, as the decision on which dosing option to choose can significantly influence a patient’s therapy adherence, treatment outcomes and total healthcare costs.
EXPLORING THE UNKNOWN IN PURSUIT OF ANSWERS
Recently, Ypsomed sought to answer these questions and studied how patient characteristics and treatment attributes influence their preferences for large-volume autoinjectors over prefilled handheld devices.1 The study surveyed 191 patients with prior self-injection experience who suffer from chronic conditions such as arthritis, asthma or cancer. The online questionnaire captured patient characteristics and asked them to complete pairwise device choice tasks expressing their preference between handheld autoinjector and wearable large-volume injector dosing options. The survey assessed various patient characteristics, such as quality of life, dexterity impairment or skin irritation, using well-established standardised scales. The research design intentionally varied treatment attributes among these choice tasks – including injection duration and frequency, perceived pain and skin irritation – to contrast different options between the two device categories and unveil tipping points where device preferences changed.
DEVICE PREFERENCES DIFFER BETWEEN PATIENT GROUPS
The study asked patients to choose between two different injection devices: a handheld autoinjector for a weekly injection that causes mild pain and skin irritation or a wearable large-volume injector for a monthly injection that causes mild-to-moderate pain and skin irritation. Figure 2 illustrates the data on injection device preference by disease area. Around one-third (31.6%) favoured the large-volume wearable injector over the handheld autoinjector. Although the overall choice for this scenario remained with the handheld device, patient groups showed differences in preference. In the healthy control group, 36.4% of the participants preferred the wearable large-volume device – but this varied from 21.9% to 42.9%, depending on the chronic disease diagnosed. Notably, patients with multiple sclerosis were most likely to prefer the wearable device, while those with psoriasis were least likely.
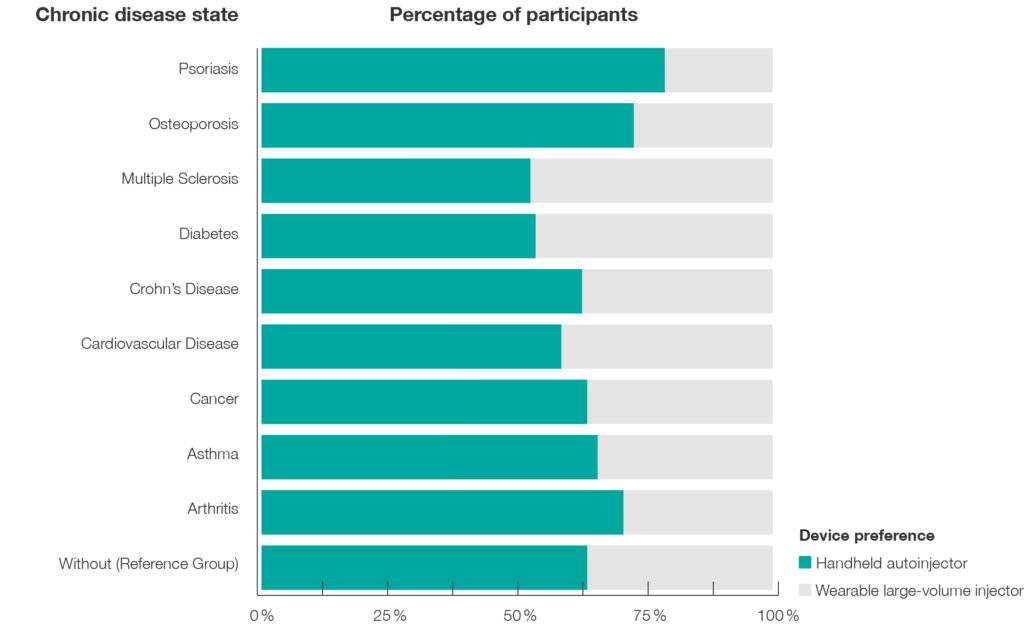
Figure 2: Device preference based on diagnosed disease state. Note: Comparison of a three-minute, weekly injection with a handheld autoinjector with a 33-minute, monthly injection with a large-volume wearable device.
“The study revealed a remarkable synergistic effect between injection frequency and duration on device preference.”
EFFECTS OF INJECTION FREQUENCY AND DURATION ON PREFERENCES
Of particular interest were the effects of changing injection frequency and duration – two critical attributes of injection-based therapies. The study advanced the critical insight that stepwise decreases in injection frequency and time significantly increased the likelihood that patients preferred the emerging category of wearable large-volume devices to market-proven autoinjectors. Patients were more likely to choose a wearable large-volume injector when reducing its injection duration from more than 30 minutes to less than ten minutes, and injection frequency from biweekly to quarterly administration.
The results of this study have significant implications for drug product development. The study revealed a remarkable synergistic effect between injection frequency and duration on device preference. In fact, over two-thirds of participants preferred the large-volume wearable device when reducing injection duration to eight minutes and frequency to quarterly injections, compared with the well-established once-weekly injection using autoinjectors. Figure 3 illustrates these effects and highlights the critical inflection point where the overall preferences shift from handheld autoinjectors to wearable large-volume devices.
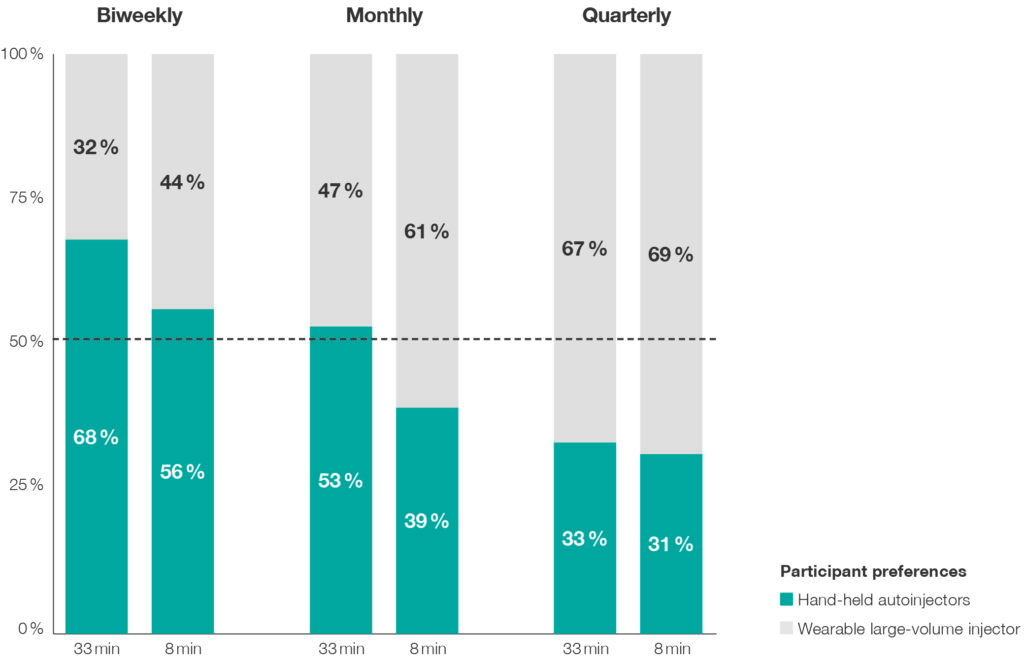
Figure 3: Device preference based on varying wearable large-volume injector injection duration and frequency. Note: The handheld autoinjector had a fixed injection duration of three minutes and a weekly injection frequency.
These findings underscore the importance of focusing on new formulations and device technologies that enable high-rate subcutaneous injections. For example, researchers may use innovative wearable large-volume injectors to accelerate the subcutaneous delivery of a drug co-formulated with permeation enhancers. By doing so, innovators can shift overall patient preferences and boost the commercial success of subcutaneously self-injected drugs.
“Patient quality of life seems to mask other individual-level characteristics on dosing preferences, such as dexterity limitations, injection experience, age or sex.”
WHY PATIENT QUALITY OF LIFE MATTERS IN CHOOSING INJECTION DEVICES
Deciphering the key drivers of patient dosing preferences is complex, as they are multifaceted and can change throughout therapy. However, the study revealed that patients with high quality of life tend to favour more frequent but shorter injections using handheld autoinjectors rather than less frequent but more prolonged drug self-administration using wearable large-volume injectors. These findings suggest that patients with better physical health find slower injections using wearable injectors attached to the abdomen or thigh more disruptive and may prefer a device that empowers them to be in full control of the process. In contrast, patients with lower quality of life appreciated the hands-free operation, automated injection process control and additional reassurance offered by wearable injectors. Notably, patient quality of life seems to mask other individual-level characteristics on dosing preferences, such as dexterity limitations, injection experience, age or sex (see Figure 4 for an overview).
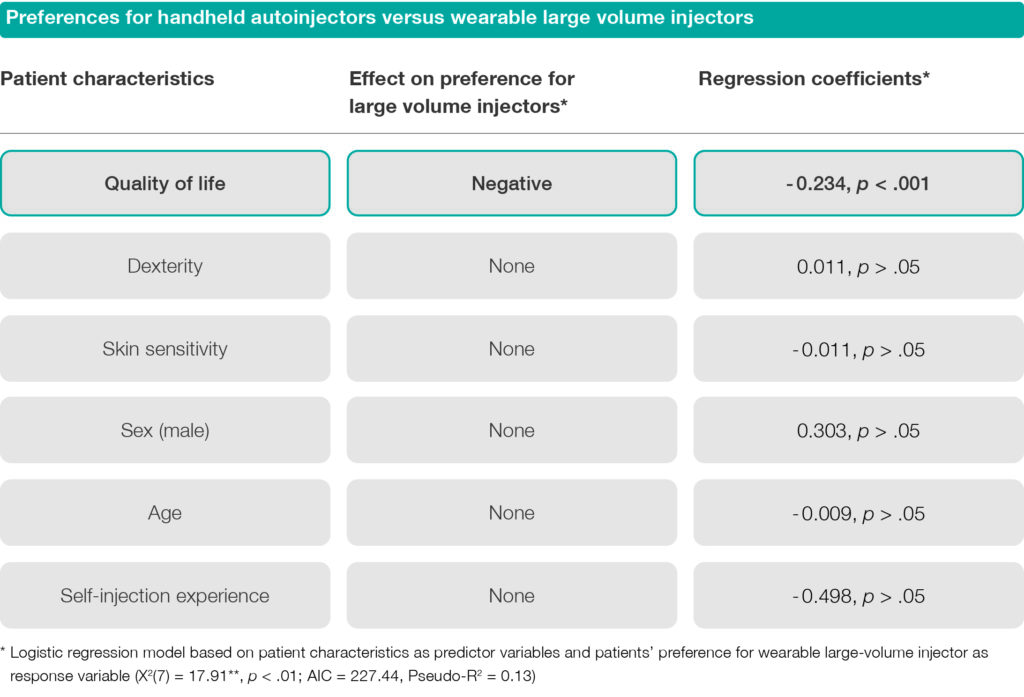
Figure 4: Effects of patient characteristics on preferences for large-volume wearable injectors.
These insights are essential for selecting and prescribing injection-based therapies for patients. By considering a patient’s quality of life and treatment preferences, healthcare providers can work with patients to choose the optimal self-injection device for their needs. Given these findings, let us return to Patricia’s case and see how her cardiologist helps her navigate this decision. He understands that patient quality of life is crucial in choosing the optimal device, so he asks about her daily activities, her overall health and how it affects her daily life.
Patricia shares that she enjoys being active and social but sometimes struggles with joint pain that limits her mobility. She also mentions that she values independence and prefers not to rely on others for help. Her doctor notes these critical factors and advises Patricia that a handheld autoinjector with shorter, more frequent injections may be the better option for her, given her desire for independence and an active lifestyle. He reminds her that adherence is vital to achieving optimal health outcomes and encourages her to follow up with him regularly to monitor progress and adjust the treatment plan as needed.
About the Study
Ypsomed, a leading manufacturer of self-injection systems for subcutaneous drug delivery, collaborated with HFC Human-Factors-Consult (Berlin, Germany) to conduct the empirical study presented in this article. As part of its commitment to advancing new insights relevant to both industry and academia, Ypsomed has established a scientific research and communications programme. The outcomes have been published in leading peer-reviewed scientific forums such as Expert Opinion on Drug Delivery, Patient Preference & Adherence and Medical Devices: Evidence and Research, and have also been presented at significant medical device and drug delivery meetings, such as PDA’s Universe of Pre-Filled Syringes and Injection Devices Conference.
REFERENCE
- Schneider A et al, “Understanding patient preferences for handheld autoinjectors versus wearable large-volume injectors”. Expert Opin Drug Deliv, 2023, Vol 20(2), pp 273–283.

