To Issue 167
Citation: Cuevas Brun EH, Chen Y, “Improving Aerosol Delivery: Nanosuspension and Mesh Technology”. ONdrugDelivery, Issue 167 (Nov 2024), pp 10–14.
Edgar Hernan Cuevas Brun and Yuchi Chen discuss how the combination of Formosa’s APNT formulation technology and HCmed’s AdheResp smart breath-actuated mesh nebuliser can work together to offer significant benefits to the aerosolisation of difficult solution-based formulations for inhalation.
“Mesh nebulisers have been proven to be effective when nebulising not only solutions but also biologic formulations due to the mild-to-negligible heat and shear forces generated by the mesh system.”
Aerosolisation of suspension-based formulations with mesh nebulisers has long been reported to be a challenging process due to the intrinsic interaction of the device and formulation. Suspension-based formulations are characterised by the heterogenous mixture of APIs in aqueous systems, driven by the drug’s low solubility.1 With inhaled formulations, suspensions are commonly micronised, therefore containing drug particles with diameters ranging in the low single-digit microns.
Active mesh nebulisers are delivery systems that turn liquid medications into an aerosol via a mechanism that uses a mesh membrane containing thousands of openings in its surface. This allows the liquid to be pushed through the pores when the membrane oscillates. Commonly, the mesh pore size is below 5 μm, with the aim of generating droplets that can travel through the respiratory airways and reach the deep lung.
Mesh nebulisers have been proven to be effective when nebulising not only solutions but also biologic formulations due to the mild-to-negligible heat and shear forces generated by the mesh system, especially when compared with ultrasonic and jet nebulisers, respectively. However, for suspensions with APIs that have a diameter close to the mesh pore size and an amorphous shape, drug delivery can be significantly affected. It has been reported that, when assessing the dose of suspension-based formulation delivered with mesh technology, a large amount of the API is retained in the medication container, as the API could not pass through the mesh pores.2
ALTERNATIVES FOR FORMULATING LOW-SOLUBILITY DRUGS
Nowadays, to resolve the issue related to insoluble or low-solubility APIs, formulation developers can opt for a number of platforms that aim to facilitate the delivery of these drugs in an aqueous environment. Some of the existing approaches are:
- Liposomes: Spherical vesicles composed of a phospholipid bilayer that are capable of encapsulating both hydrophilic and hydrophobic drugs. These are characterised by their high biocompatibility and tuneable drug-release rates.3
- Polymeric or Inorganic Nanoparticles: Nanoparticles designed to encapsulate drugs by unique surface modification properties. These methods, which may employ materials such as polymers, silicon or gold, allow for imaging, phototherapy, targeted drug delivery, controlled release and protection of the drug from degradation.4
- Solid Lipid Nanoparticles: Nanoparticles made of solid lipids that can encapsulate drugs, offering high physical stability and good biocompatibility.5
- Micro- and Nano-Emulsions: dispersions of oil and water phases into micron- or nanometre-sized droplets, characterised by simple preparation and high stability, that can improve drug solubility.6
- Nanocrystals: Conventional drug particles mechanically milled to a sub-micron scale, providing simple and scalable production process compared with other nanocarrier systems. The milling uses foreign agents, such as metal and plastic beads, which may result in the issue of media detachment and residue in the final product, thereby presenting a difficult purification process.
Some of these approaches can be used for inhaled suspension-based formulations; however, for platforms that are suitable for producing inhaled formulations, additional assessment of delivery with mesh nebulisers must be assessed. Physicochemical properties such as viscosity, surface tension and osmolality, which may be associated with the API concentration in the formulation, may also impact the delivery performance and efficiency.
“By reducing particle size in a novel fashion, APNT enhances the dissolution and bioavailability of poorly soluble APIs while providing a homogeneous and aqueous-based nanosuspension formulation with excellent stability.”
AN INTRODUCTION TO APNT
The Active Pharmaceutical (ingredient) Nanoparticle Technology (APNT™) formulation platform, a proprietary and patented formulation platform of Formosa Pharmaceuticals, uses particle size reduction to enhance drug dissolution and bioavailability while minimising contamination risk. As the pharmaceutical industry continually seeks innovative methods to improve drug delivery and efficacy, the APNT formulation technology introduces a significant advancement in the field. By reducing particle size in a novel fashion, APNT enhances the dissolution and bioavailability of poorly soluble APIs while providing a homogeneous and aqueous-based nanosuspension formulation with excellent stability.
APNT uses common salts and sugars as milling media. Following milling, these media can remain part of the final formulation, eliminating the need for the isolation or purification of the API from foreign objects that is often required by other platforms. As a result, the process is streamlined and has a lower risk of contamination. The technology allows for precise tuning of particle size, from low micrometre down to sub-100 nanometre ranges, optimising application and penetration efficiency. The key advantages of APNT are shown in Figure 1.
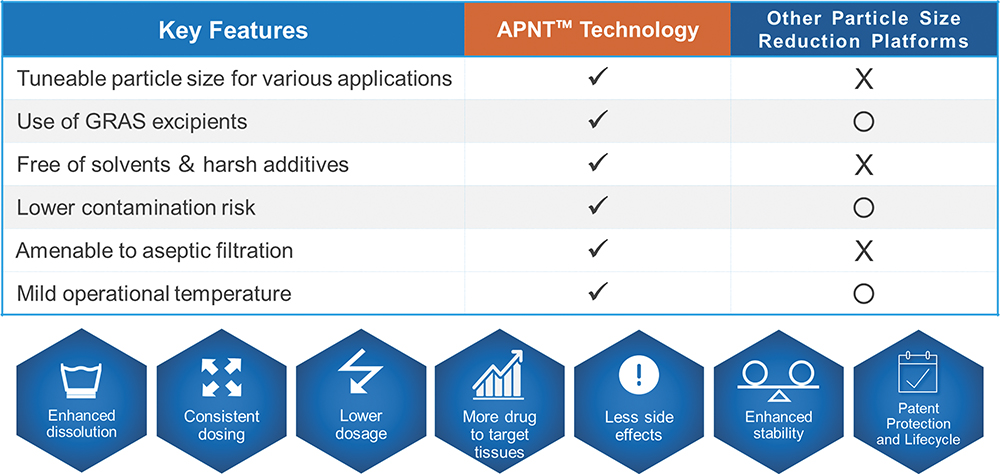
Figure 1: APNT key advantages.
APNT is versatile and suitable for various administration routes, including oral, inhaled, topical and ophthalmic applications. It has been successfully applied to small-molecule APIs across a wide range of chemical classes and therapeutic indications. This technology has been validated in Formosa Pharmaceuticals’ US FDA-approved clobetasol propionate ophthalmic suspension 0.05% (APP13007), a multidose eye drop for the treatment of postoperative inflammation and pain following ocular surgery.
ADVANCED MESH NEBULISERS – DELIVERY OF SUSPENSIONS

Figure 2: The AdheResp smart breath-actuated mesh nebuliser.
Advancements in mesh technology, as well as the introduction of innovative features, have placed mesh nebulisers at the front and centre of delivery system options for inhaled combination products. Furthermore, the customisation capabilities offered by mesh nebuliser platforms enable pharmaceutical companies to tailor the drug-nebuliser match to achieve optimised levels of delivery efficiency while also improving usability options.
The smart breath-actuated mesh nebuliser AdheResp® (Figure 2) – designed, developed and manufactured by HCmed Innovations – presents a highly customisable platform that provides solutions to fulfil aerosol performance and usability requirements. The AdheResp nebuliser has been shown to deliver formulations that range from bronchodilator solutions to inhaled corticosteroids and biologics effectively.7 Some of the platform’s key features that add extra value are:
- Breath Actuation: This significantly enhances drug delivery by only aerosolising during a fraction of the inhalation phase. It also reduces the emission of fugitive aerosols that would otherwise expose bystanders to unwanted aerosol. Consequently, lower amounts of formulation are needed to achieve the same dose than when delivering with continuous output nebulisers, which can be significantly beneficial for high value drugs, such as biologics.
- Bluetooth Connectivity: This enables the transmission of data in real-time or later transmission to a mobile app for distribution via medical clouds. The goal is to facilitate data sharing between patients and medical practitioners to monitor patient adherence and provide treatment guidance.
- Activation System (Lock-and-Key): The inclusion of an activation system can serve as an option to bond the formulation to a specific device. This feature ensures that the drug is delivered with the intended dose and aerosol characterisation, as the nebuliser is customised to optimise the drug-nebuliser performance.
- Guidance Options: Nowadays, appropriate guidance during inhalation is widely considered important for usability feedback. This can take various forms, including visual, tactile and acoustic, as well as making use of the Bluetooth connectivity function.
Nonetheless, when it comes to the delivery of suspensions, platforms such as the AdheResp mesh nebuliser may still be affected by micro-sized particles that cannot easily pass through the mesh pores due to their large and amorphous characteristics. For this reason, formulation and device tailoring are equally important to achieve the expected performance. As a result, opting for nanosuspension formulations could be a more suitable approach for delivery via mesh technology.
NANOSUSPENSIONS AND MESH TECHNOLOGY – CASE STUDY
For a study with the aim of gaining a better understanding of the influence of different suspension particle sizes when delivering with a mesh nebuliser, a well-known macrolide antibiotic was selected as the API (water solubility: 0.33 mg/L). APNT was applied to produce two formulations with particle sizes of D90 <250 nm and <800 nm at concentrations of 3.0 and 2.8 mg/mL, respectively. The AdheResp breath-actuated mesh nebuliser aerosolised the formulation using a modified main unit for higher driving power and four reservoirs with the same specifications (two reservoirs for each formulation). The decision to select a modified main unit was determined by the physicochemical properties of the formulations in the range of 1.30 cP for viscosity and 43 mN/m for surface tension. These values present a slightly higher viscosity and lower surface tension compared with water.
Aerosol characterisation was conducted using a laser diffraction particle size analyser (Spraytec, Malvern Panalytical), which was connected to a system operating with a pump at 15 L/min. The delivered dose and treatment time were computed by delivering 2 mL of each formulation when using a breath simulator (BRS 200i, Copley Scientific, UK), operating according to the configuration stated in USP <1601> for the adult breathing pattern. High-performance liquid chromatography analysis was performed to quantify the API of the collected samples. All tests with the corresponding reservoirs were conducted in three replicates and the mean values are summarised in Table 1.
| Laser Diffraction Analyser | Breath Simulator | ||||
| Antibiotic Formulation (Particle Size) |
Dv50 (μm) |
Fine Particle Fraction (%) |
Geometric Standard Deviation | Delivered Dose (mg) |
Treatment Time (mm:ss) |
| D90 <250 nm | 4.38 | 58.91 | 1.72 | 4.21 | 9:44 |
| D90 <800 nm | 4.21 | 61.01 | 1.77 | 3.77 | 10:32 |
Table 1: Mean values for aerosol characterisation and delivered dose studies (n = 3).
The results of the study showed an increase in treatment time and decrease in delivered dose for the D90 <800 nm formulation (Figure 3). There was a significant difference when comparing the delivered dose of the formulations (p <0.05, p = 0.01). These observations could be directly associated with the larger nanosuspension particle size. With the droplet size distribution, the Dv50 of the D90 <250 nm formulation was slightly larger than the D90 <800 nm formulation, which, in this case, could be an artifact of the higher output rate, which may have led to a higher chance of collision between droplets during aerosolisation. Nonetheless, the delivery of both formulations was close to 70% of the loaded API, showing the efficient performance that resulted from the pairing of a breath-actuated mesh nebuliser and two nanosuspension formulations.
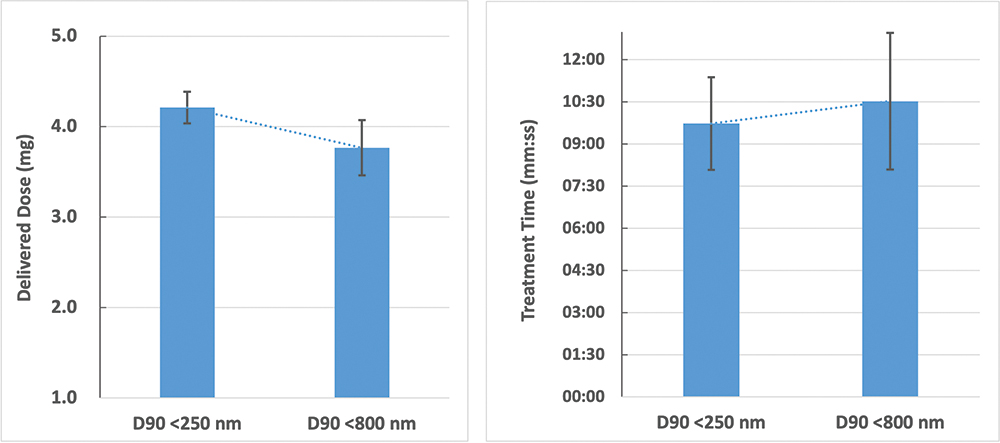
Figure 3: Trend in delivered dose and treatment time for delivery of nanosuspensions.
CONCLUSION
Understanding device–formulation interactions is fundamental for improving delivery performance. Customisation of the device and formulation to create a more suitable pairing can be exemplified in the combination of a breath-actuated mesh nebuliser and nanosuspension formulation, overcoming the previously documented challenges of delivering suspensions with mesh technology.
The capability to enhance drug delivery efficiency and maintain efficacy with lower dosages provides a valuable tool in the development of drug-nebuliser combination products. As shown more specifically in the case study, it was observed that the combination of Formosa Pharmaceuticals’ APNT formulation technology offering a novel approach to drug delivery through particle size reduction with HCmed’s AdheResp smart breath-actuated nebuliser increases delivery of the API by significantly reducing aerosol loss during each breathing cycle. APNT and the AdheResp platform are powerful options that can provide a significant contribution to the inhalation field when combined. Together, they hold the potential to significantly improve therapeutic outcomes and patient experiences in existing and future therapies.
REFERENCES
- Pinar SG et al, “Formulation Strategies of Nanosuspensions for Various Administration Routes”. Pharmaceutics, 2023, Vol 15(5), article 1520.
- Elphick M et al, “Factors to consider when selecting a nebulizer for a new inhaled drug product development program”. Expert Opin Drug Deliv, 2015, Vol 12(8), pp 1375–1387.
- Gregoriadis G, “Engineering liposomes for drug delivery: progress and problems”. Trends Biotechnol, 1995, Vol 13(12), pp 527–537.
- Croy SR, Kwon GS, “Polymeric micelles for drug delivery”. Curr Pharm Des, 2006, Vol 12(36), pp 4669–4684.
- Müller RH, Mäder, Gohla S, “Solid lipid nanoparticles (SLN) for controlled drug delivery – a review of the state of the art”. Eur J Pharm Biopharm, 2000, Vol 50(1), pp 161–177.
- Jafari SM, McClements DJ, “Nanoemulsions: Formulation, Applications, and Characterization”. Academic Press, 2018, pp 3–46, 104–346, 415–433.
- Cuevas Brun EH et al, “Aerosol Delivery Performance of Interferon Beta-1b with a Continuous Output Mode Mesh Nebulizer and a Breath-Actuated Mesh Nebulizer”. Resp Drug Deliv, 2022, Vol 2022, pp 235–240.

