To Issue 160
Citation: Clement J, Welch B, “Accelerating Innovation: The Power of Parallel Development for an Autoinjector Launch”. ONdrugDelivery, Issue 160 (May 2024), pp 21–24.
Jeff Clement and Bill Welch of PCI Pharma Services explore the essential considerations for navigating the parallel development of a drug product in a vial and a prefilled syringe for an autoinjector, together with the downstream final assembly and pack considerations, from early-phase clinical trials to commercialisation.
The journey from early-phase clinical trials to successful commercial launch for an injectable drug product is complex and multifaceted. When considering the delivery system, the choice between a traditional vial or prefilled syringe (PFS) and a modern autoinjector can significantly impact the patient experience, adherence and market competitiveness. Parallel development of both vials and PFSs for autoinjector options requires careful consideration to ensure regulatory compliance, patient safety and commercial success.
“Data gathered and analysed during parallel container studies in early clinical trials eases the transition to PFSs for later-phase clinical trials.”
PRECLINICAL AND EARLY-PHASE TRIALS
Traditionally, for intravenous (IV) administration of a drug product, either a single or multi-use vial would be the primary container of choice for biopharmaceutical companies during preclinical and early-phase clinical trials. With the primary objectives being proof of concept, safety and tolerated dose, vials present a high degree of flexibility with respect to fill volume and applied dose, supporting the immediate need for speed through the clinic.
However, with the modern focus on patient centricity and the increasing adoption of self-administration devices across various therapeutic areas for anaphylaxis, allergies and chronic diseases such as psoriasis, diabetes, multiple sclerosis and rheumatoid arthritis, biopharmaceutical companies are actively incorporating patient-viable subcutaneous (SC) dosage forms, such as PFSs and autoinjectors, into their product portfolios. Due to companies recognising the competitive advantage these devices offer in terms of differentiation, patient compliance and patient satisfaction, the autoinjector market is witnessing a surge in innovation. Biopharmaceutical companies are not only investing in research and development to enhance device features and compatibility with a diverse range of large- and small-molecule drug products, but they are also introducing and evaluating them as viable dosage forms earlier in clinical trials.
BALANCING THE IMMEDIATE WITH THE FUTURE: PARALLEL DEVELOPMENT
Changing the method of administering a treatment during clinical trials, such as changing from IV to SC delivery and introducing a combination product, brings added complexity to both technical and clinical development plans. This necessitates additional clinical bridging studies, including assessments of bioavailability and safety, as well as technical comparability studies if adjustments are made to the concentration, pH, tonicity or other critical quality attributes of the formulated drug product, which will add time and cost to the development programme. To address these challenges, biopharmaceutical companies are looking to parallel development strategies.
Parallel development in early-phase clinical studies involves concurrent and co-ordinated advancement of both drug and container/device components from early stages through to commercialisation. With the key objective of accelerating time to market, close collaboration between pharmaceutical development and injectable device packaging teams is essential to align goals and streamline processes.
CONTAINER CLOSURE STUDIES
Parallel container studies are conducted during the development of drug products to compare the performance, stability and compatibility of the product when packaged in different container types. Evaluating multiple container closure system configurations early in the development lifecycle provides optimum flexibility and accelerates speed to market.
Specifically, when considering drug products packaged in vials versus PFSs, parallel container studies aim to assess any differences in factors such as stability, container-material interactions, drug product integrity and usability. These studies involve packaging the same formulation of the drug product into both vials and PFSs and subjecting them to a series of tests and evaluations. The following tests are some key aspects of parallel container studies for drug products in vials and PFSs.
Stability Testing
Both vials and PFSs are subjected to stability testing under various storage conditions (e.g. temperature, humidity) to evaluate the degradation kinetics of the drug product. This helps determine whether there are any differences in stability between the two container types. Putting both vials and PFSs down for stability during early-phase trials provides access to more than two years of stability data compared with beginning only with a vial format. So, even if clinical trials are being conducted using a vial, stability data is being collected simultaneously on PFS presentations, buying time for later-phase trials.
Similarly, autoinjector functional stability tests following ISO 11608-5, such as cap removal force, activation force, extended needle length, dose accuracy, injection time and lockout force, can be conducted in parallel, saving valuable time should a decision be made in later-phase trials to proceed with this method of drug delivery.
Container-Drug Product Interaction Studies
These studies assess the compatibility of the drug product with the materials used in vials and PFSs. They aim to identify any interactions between the drug product and the container that could affect product stability, efficacy or safety. Photo-stability studies should also be initiated to evaluate drug product sensitivity to light.
The most critical aspect of primary packaging is for it to be as inert as possible so that it does not react with, add to, absorb or allow external factors to change a drug product’s established safety, strength, quality, stability or purity characteristics. The material must be chemically stable, support the required concentration of the drug, not cause any extractables or leachables issues and not delaminate or undergo other changes upon contact with the drug product.
Container Closure Integrity Testing
Container closure integrity (CCI) is critical for maintaining the sterility and stability of the drug product. Both vials and PFSs undergo testing to ensure that the container closure system combination effectively prevents contamination and leakage. CCI testing may be conducted in parallel with autoinjector functional stability testing.
Usability and Human Factors Studies
Parallel studies may also include assessments comparing usability and patient preference between PFSs and autoinjectors. Factors such as ease of handling, convenience and patient comfort are evaluated to determine which container type may be preferred by end users. With a focus on patient centricity, assessing the interaction between users and the product, as received, is paramount. Understanding how patients and healthcare professionals interact with the packaging, instructions for use (IFU) and the device itself is vital for optimising usability, minimising user errors and enhancing overall safety, efficacy and adherence to achieve improved outcomes (Figure 1).
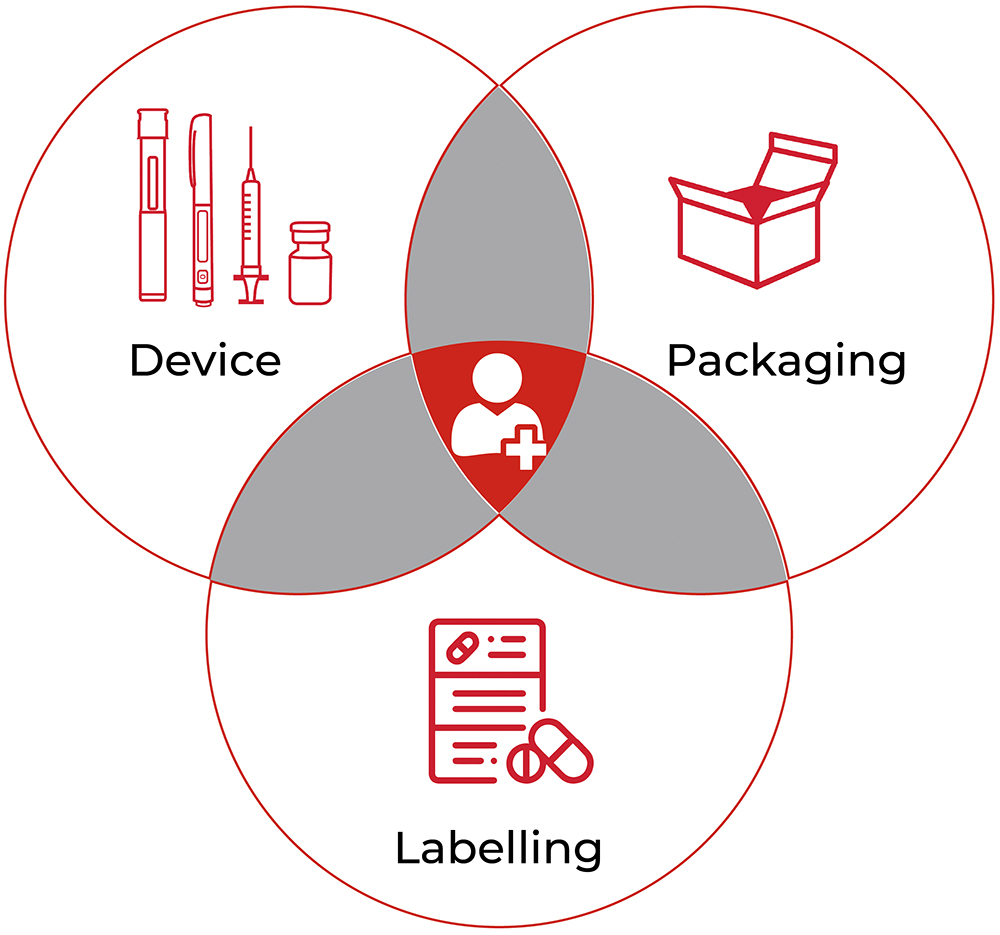
Figure 1: Patient experience = device + packaging + labels/IFU.
Conducting usability studies and incorporating human factors considerations early in the design process can help identify potential issues and inform design modifications. Human factors and usability engineering is an integral component of regulatory submissions and is essential for demonstrating a product’s usability and user comprehension.
Regulatory Considerations
Parallel container studies are conducted in compliance with regulatory guidelines, which may vary depending on the geographic region. Regulatory authorities require comprehensive data demonstrating the comparability and suitability of both container types for the intended drug product.
“From early-phase clinical trials to successful commercial launch, considerations such as drug product device compatibility, manufacturability and packaging design must be carefully navigated.”
BENEFITS OF PARALLEL DEVELOPMENT
The benefits of parallel development include:
- Expedited Timeline: Running drug and device development activities in parallel can significantly reduce the overall time to market by eliminating sequential processes and optimising workflows.
- Enhanced Efficiency: Co-ordinated efforts and shared resources can lead to improved efficiency in development activities, resulting in cost savings and faster decision making. Streamlining processes and workflows can lead to improved efficiency in resource use and decision making.
- Regulatory Alignment: Aligning regulatory strategies for both drug and device elements early in the development process facilitates smoother regulatory approval and market entry.
- Cost Savings: eliminating redundant activities and optimising resource allocation can result in overall cost savings throughout the development lifecycle.
Parallel container studies provide valuable insights into the performance of drug products in vials and PFSs, helping biopharmaceutical companies make informed decisions regarding primary packaging choices based on factors such as stability, compatibility and patient preferences – avoiding costly delays on the journey to commercialisation.
DRUG-DEVICE STRATEGY
Data gathered and analysed during parallel container studies in early clinical trials eases the transition to PFSs for later-phase clinical trials. Typically, in Phase IIb clinical trials, biopharmaceutical companies seek to make decisions on the therapy’s drug-device strategy – whether to continue with the PFS as is, convert to a needle safety device or insert it into an autoinjector to provide ultimate flexibility for various healthcare professionals, patient populations or reimbursement schemes.
Considering the target product profile and quality target product profile, decisions can be made on whether there is a unique need for device innovation for specific patient populations or if traditional, readily available platforms would be suitable. Selecting established platforms that have already received regulatory approval as part of a drug-device combination product may be deemed lower risk for a new programme (Table 1).
| Advantages | Disadvantages | |
| Established platform |
|
|
| Proprietary platform |
|
|
Table 1: The advantages and disadvantages of established versus proprietary platforms.
PACKAGE DESIGN FOR MANUFACTURABILITY
To avoid unnecessary delays and additional costs, consultation between developers and clinical and commercial stakeholder groups is important throughout the parallel development lifecycle. Packaging design is a critical area of importance, so early consideration of manufacturability is encouraged. Considering package design earlier in the drug development process can lead to both cost and time efficiencies as the cost of mistakes can be considerable and delay product launch milestones. By ensuring that design and operational teams work together and apply a design for manufacture philosophy, the team swill understand the impact of design on packaging operations earlier in the process, delivering a streamlined and longer-term efficient solution.
A common challenge often arises when a biopharmaceutical company has had its packaging designed by a third-party design agency, which may fit the end-user specification and sponsor’s branding requirements but does not fit on existing packaging infrastructure when it comes to commercial manufacture. A design that is not optimised for the packaging process equipment will result in unnecessary upfront capital costs, modifications to existing equipment and higher labour and commercialisation costs, ultimately resulting in higher manufacturing costs and lower commercial revenues.
BEST PRACTICES AND STRATEGIES
With many critical considerations when conducting parallel development of a novel drug product in vials and PFSs for autoinjectors, there are several best practices that can help ensure a smooth and efficient process, including:
- Early Collaboration: It is important to establish cross-functional teams of all stakeholders involved in the development process, including formulation scientists, packaging engineers, regulatory experts, quality assurance professionals and patient focus groups. Fostering collaboration and communication from project initiation ensures alignment of goals, troubleshooting and efficient progress.
- Risk Management: Proactively identifying and addressing potential risks, such as technical challenges or regulatory hurdles, can help mitigate delays and ensure project success.
- Iterative Development: Embracing an iterative approach allows for continuous refinement and optimisation based on user testing, regulatory feedback and market insights.
- Regulatory Compliance: It is critical to ensure compliance with regulatory requirements for vials, PFSs and autoinjectors in the target markets. This includes adherence to relevant guidelines for drug product packaging, device design, quality control and documentation.
- Flexibility and Adaptability: Maintain flexibility and adaptability throughout the development process to accommodate any unforeseen challenges or changes in project requirements. Be prepared to adjust timelines, resources and strategies as needed to optimise the parallel development of vials and PFSs for autoinjectors.
CONCLUSION
Parallel development has emerged as a strategic approach to expedite the development process and bring innovative therapies in drug-device combination products, such as autoinjectors, to market faster. From early-phase clinical trials to successful commercial launch, considerations such as drug product device compatibility, manufacturability and packaging design must be carefully navigated. By addressing these considerations proactively and strategically, biopharmaceutical companies can streamline their clinical to commercial process and, ultimately, improve patient outcomes.
To find out more about PCI Pharma Services and the development of combination products, visit: pci.com.

