Citation: Quint J, “A New Mindset for Combination Product Development”. ONdrugDelivery, Issue 125 (Oct 2021), pp 35–38.
Jennifer Quint offers insights into how to plan and execute technology transfer effectively, explaining Pfizer CentreOne’s three-phased approach that can successfully support this pivotal event in a drug product programme’s journey to commercialisation.
Central to every commercial relationship with a contract development and manufacturing organisation (CDMO) is the technology transfer. A number of subject matter experts from both the sponsor and the CDMO may be involved in developing and manufacturing a product, making the technology transfer process both complex and critical to success.
“With sterile injectables, both the SU and the RU need to gather additional information – and do so as early in the process as possible.”
Many organisations have their own definition of what constitutes a technology transfer, but the US FDA points to ICH Q10, “Guidance for Industry Q10 Pharmaceutical Quality System” published in 2009, to define its guidance. “The goal of technology transfer activities”, the guidance states, “is to transfer product and process knowledge between development and manufacturing, and within or between manufacturing sites to achieve product realisation. This knowledge forms the basis for the manufacturing process, control strategy, process validation approach and ongoing continual improvement.”
As explained in ICH Q10, this internationally harmonised guidance is intended to help pharmaceutical manufacturers by describing a model for an effective quality management system. It is a systematic, logical procedure that transfers the documented knowledge and experience gained during chemistry and formulation development to an appropriate, responsible and authorised commercial manufacturing entity.
A priority for many sponsors, therefore, is finding partners with the specific scientific and technical capabilities to transfer their formulation chemistries from a source unit (SU) to the commercial-scale receiving unit (RU) in compliance with regulatory guidance. All successful technology transfers require discipline and collaboration. However, when it comes to the aseptic finishing and filling of sterile injectable therapeutics, obtaining this base knowledge can present specific challenges (Figure 1).
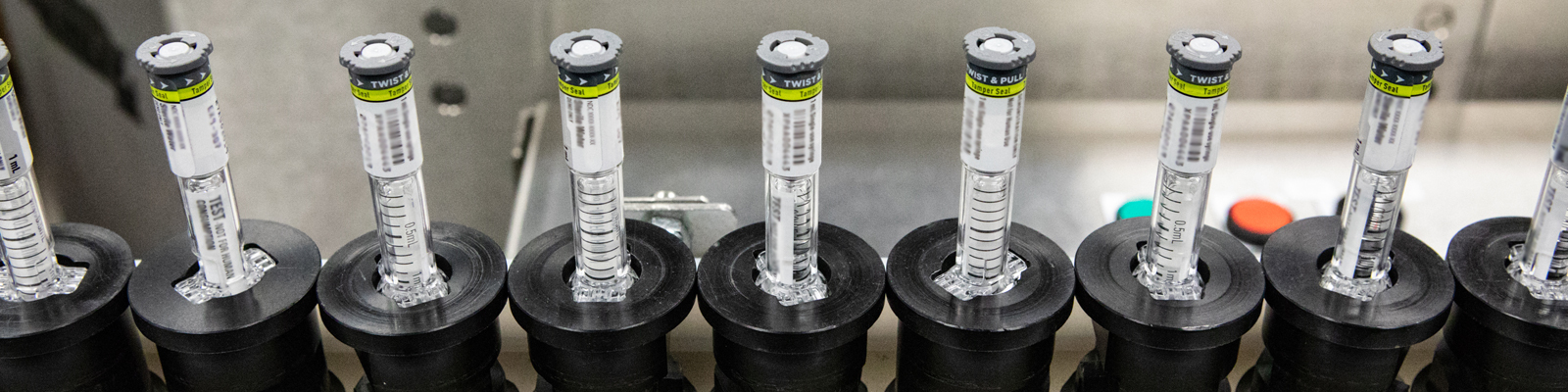
Figure 1: Technology transfer is never a simple process, but there are additional challenges when dealing with sterile products such as injectable therapies.
START A WELL-DEFINED SCOPING PROCESS
With sterile injectables, both the SU and the RU need to gather additional information – and do so as early in the process as possible. The earlier a well-defined discovery begins, the better it will be at communicating and transferring the main agenda of the drug programme. Four key considerations should feature prominently when scoping sterile injectable technology transfer:
1. Geography
The location of the RU may impact the completion of a compliant, efficient technology transfer, as changes that are permissible in one jurisdiction may not be allowed in another due to the regulatory environments in which they operate.
2. Compliance
Although compliance is a broad term, a “compliant” technology transfer begins with a careful evaluation of the applicable regulatory guidance that pertains to a product’s finished commercial state. For example, more mature commercial product transfers may see more compliance challenges in the dossier and equipment/facility contemporisation.
3. Technical
Sterile injectables are typically considered to be a high-risk product, in large part due to the duration of a drug development project. Sterile injectables can take 2–10 years to move from Phase I clinical trials to full commercialisation. Such a project is prone to outside factors, such as regulatory changes (e.g. nitrosamines, elemental impurities) or supplier changes, impacting the overall project scope and timeline. Defining the technical bases and outlining process elements should be a part of early discovery and a critical dialogue that sets the stage for a more formal technology transfer process.
4, Project and Site Talent
It is also critical to engage with the CDMO’s core team and subject matter experts early and to continue to ask questions throughout the process. As with any aspect of drug development, a technology transfer can only be successful if all teams actively work together from the start.
PICK THE PROFESSIONALS AND ALIGN ROLES
When a sterile injectable technology transfer project involves multiple partners, additional protective measures are called for. Before actual due diligence is conducted, there should be a confidentiality agreement signed and in place. Programme managers and sponsors should both know that, throughout the drug development programme, all project information and data must remain confidential and secure.
Role alignment is another tactic that supports a successful technology transfer. All outcomes should be documented on an ongoing basis, such as having a comprehensive product transfer plan (PTP), so that a mutual understanding is shared across all team members and stakeholders from the beginning of the project to the very end.
THE THREE PHASES OF A SUCCESSFUL STERILE INJECTABLE TECHNOLOGY TRANSFER
“Conducting a deep dive and thorough assessment of gaps between the SU and the RU can help the project team understand, document and manage the risks associated.”
In most “lessons learned” shared among sponsors and commercial partners, the common reasons for technology transfer failure include:
- Not anticipating the impact of changing facility or equipment (batch failures)
- Not anticipating the new regulatory environment or requirements (scope creep)
- Tacit knowledge of the product not captured or transferred to the partner or RU.
Taking a systematic approach during the scoping phase of technology transfer is important. Conducting a deep dive and thorough assessment of gaps between the SU and the RU can help the project team understand, document and manage the risks associated.
Pfizer CentreOne, defines three key phases of a technology transfer (Table 1):
| Phase One – Define and Scope | Phase Two – Plan | Phase Three – Execute | |
| Key Success Factors | • Knowledge gathering • Gap analysis • Risk assessment |
• Establish project schedule • Check and optimise • Have a risk management plan |
• Collect project data • Analyse variance • Mitigation plans • Communicate project progress |
Table 1: Pfizer CentreOne defines three phases that are a key part of any successful technology transfer.
PHASE ONE – DEFINE AND SCOPE
Phase One defines the scope of the project and helps to establish organisation and a project charter. This is accompanied by a knowledge-gathering process that encompasses the programme’s current status and future outcomes. Phase One also sets the stage for a gap analysis and failure modes and effects analysis risk assessment. Lastly, long lead-time items are covered, and the transfer protocol is defined. At a high level, at the beginning of the project, it is important to define what is in and out of scope:
- What type of transfer is it – is it from development to commercialisation or is it transferring from an existing commercial site to a new one?
- What is the status of each receiving site – is it a green field site or is it GMP certified? How many receiving sites are involved in the project?
- Is this an intra-company transfer or is it an inter-company transfer?
- If an external partner is involved, what is in the contract regarding the technology transfer scope, roles and responsibilities?
- How many stock-keeping units are involved?
- What are the targeted markets in which the sponsor intends to file?
- What is the current supply chain (APIs, raw materials, excipients, etc) versus the future supply chain?
“The benefit of having a documented charter and a PTP is that it ensures that there is a shared understanding of the project and its objectives.”
Even though the teams may not have concrete answers to these questions up front, they must be asked, documented and tracked so that information stays visible and can be actioned by the team.
It is never too early to define the project charter or to work on the PTP. The benefit of having a documented charter and a PTP is that it ensures that there is a shared understanding of the project and its objectives. The project charter and PTP are also tools to facilitate project planning.
PHASE TWO – PLAN
In Phase Two, the planning stage, the CDMO’s technology transfer team will develop a work breakdown structure and outline critical milestones. This phase includes the development of the preliminary schedule and the generation of resource estimates. During this phase, the involved parties each develop their own risk management plans, refine transfer protocols, establish a clear schedule and lay the groundwork for the transition to the execution phase.
Why is Planning Important?
Not having a project schedule can lead to confusion pertaining to which stakeholder is responsible for each activity at each stage and whether the end goal of the project is still on track. Too little detail can paint an unclear picture, whereas too much detail can obscure important information. With the right amount of information, the project may be tracked and managed effectively. Ideally, every project plan should have some lag built into the schedule to accommodate any unforeseen circumstances.
Optimise Project Review Frequency
Determining the right frequency to review and, if need be, optimise project timelines and charters can be just as important as the amount of detail that is put into each document upon its creation. If managers check too infrequently, they might miss something. On the other hand, if managers review too frequently, then it may appear that the project is not moving along as it should be. Additionally, reviewing the project charter against the timeline ensures that the project goals that have been communicated to key stakeholders are in alignment with the project’s current progress.
Define a Risk Management Plan
A risk management plan can track items that were not scoped and assign a level of risk to activities that could impact the overall project timeline. Such plans also function to define the project’s overall agreed risks and provide a good communication tool when checking in with sponsors and key stakeholders. A risk management plan can help to reduce the risk of failing to file in accordance with the agreed timeline.
The risks associated with a technology transfer project include technical risk, regulatory risk and supply chain risk. Technical risk assessment, also known as a robustness assessment, employs various tools to identify the highest risks associated with the technical aspects of the technology transfer. The technical risk assessment relies on the development and manufacturing history of the product and is a documented, data-driven process.
A regulatory gap assessment handles strategies associated with various change scenarios, as well as contemporisation requirements. The outcome of the regulatory gap assessment is typically a regulatory strategy document, also known as a risk registry, which is used throughout the transfer project to communicate and manage the regulatory risks.
A supply chain risk assessment will yield a supply chain transition plan. This includes supply chain changes that might impact the robustness and regulatory assessments. The outcome of the technical and regulatory assessment will be used as the basis for the supply chain transition plan.
PHASE THREE – EXECUTE
Phase Three is an exciting milestone where the programme team tracks and manages the project and collects status data.
As operational data arrives, the programme team analyses variances and looks for adaptive actions to ensure that quality and process optimisation goals are met. Project status reporting is vital during this phase to ensure transparency and clear communication.
Depending on the complexities of the programme, weekly team meetings and sometimes sub-meetings may be necessary to track actual progress against the established PTP and timeline. Check-ins can become even more critical when unforeseen issues arise. Working together to troubleshoot and correct issues can have a significant impact on a timeline in the long run, but might also make a process more robust.
Communication within the CDMO’s team is often just as critical as communication with programme stakeholders. All stakeholders want to know is:
- Are there any issues or emerging risks that could significantly impact the project?
- How is the programme tracking against the agreed budget and timeline?
“It is crucial to pay close attention to the transfer process, carrying out proper definition and planning prior to any execution. Failure to do so could lead to unnecessary delays and downtime, with implications for project timelines.”
FOLLOWING THE PROCESS IS CRITICAL TO PROGRAMME SUCCESS
Technology transfer is complex, particularly for sterile products. With this in mind, it is crucial to pay close attention to the transfer process, carrying out proper definition and planning prior to any execution. Failure to do so could lead to unnecessary delays and downtime, with implications for project timelines.
Working closely with the CDMO and other stakeholders from the very beginning of the definition and planning phases is an essential part of any effective transfer. Such collaboration can ensure that any potential pitfalls and risks are accounted for and mitigated against before they become a problem. It can also help all parties ensure that they have the capacity, capability and infrastructure in place ready for the project handover, helping to ensure development continues smoothly and efficiently.

