To Issue 128
Citation: Shain A, “Towards a New Standard of Care With Aptar Pharma’s Digital Health”. ONdrugDelivery, Issue 128 (Dec 2021), pp 6–9.
Adam Shain discusses how Aptar is building on the progress made in connected drug delivery devices to help realise their full potential by developing an open, end-to-end platform that will enable healthcare stakeholders to take a holistic view of the full drug delivery journey.
“Aptar Pharma believes that the future of therapeutics is best supported by an open, end-to-end platform that hosts medical devices and digital health products, alongside the services that complement and enhance them.”
The development of drug delivery devices suitable for patient self-administration was a critical step in improving the standard of care worldwide. Instead of needing to visit a hospital or clinic to receive an injectable medication or take a slow-acting pill, now patients can often administer their own therapeutics from the comforts of home.
However, this innovation represents but a single step, as early versions of drug delivery devices offered patients no insight into whether they had used them correctly or taken the right dose. To meet this need, the market for patient support tools has evolved over time, bringing connected healthcare devices, disease management programmes, digital health applications and the latest innovation of digital therapeutics.
Managing the vast quantity of data that emerges from this evolving ecosystem, and gleaning useful insights from it, has proven to be a tall order. Data silos, walled gardens and proprietary systems make it difficult to share information. This forces providers, payers, pharmaceutical companies and patients to make care decisions by looking at an incomplete picture of how patients take or respond to a particular therapeutic.
Aptar Pharma believes that the future of therapeutics is best supported by an open, end-to-end platform that hosts medical devices and digital health products, alongside the services that complement and enhance them. This belief has informed Aptar Pharma’s growth strategy, positioning the company to push the industry towards a new standard of healthcare.
FROM DEVICES TO THERAPEUTICS: HOW DRUG DELIVERY HAS EVOLVED

Figure 1: The evolution of patient support tools.
The transition from standalone analogue medical devices to digital therapeutics, powered by clinically evaluated software and validated medical guidelines, represents an ongoing evolution in healthcare delivery (Figure 1). As these patient support tools have become more sophisticated, more available, cheaper to produce and simpler to use, they have improved the standard of healthcare across the care continuum.
Physicians have used medical devices for millennia, dating back to a flint-tipped drill used some 9,000 years ago by dentists in modern-day Pakistan. Today, there are an estimated 500,000 medical devices on the market, according to “Medtech and the Internet of Medical Things: How Connected Medical Devices are Transforming Health Care“, a July 2018 report by Deloitte. One key category is drug delivery devices, covering pulmonary, nasal, ocular, injectable and dermal therapies, that allow patients to administer medications at home, without the need for assistance from a physician or nurse. These provide patients with a convenient option for getting the medication they need, when they need it. The primary downfall of early-stage drug delivery devices was a lack of real-time connectivity – patients needed to record dosing data themselves and share it with a provider over the phone or during a subsequent clinic visit.
Using wired, wireless, cellular or Bluetooth connectivity, connected devices can transmit data to a computer, standalone application or data repository. This provides a tangible record of device data, saves users from needing to record and re-enter data, and reduces the likelihood of human error from misreading the device display.
Early Connected Devices
Unfortunately, early versions of connected devices ported data to standalone silos, making it difficult to share with clinical applications. Furthermore, simply seeing rows and columns of numbers in a database left clinicians and patients without the context that is critical for informed decision-making.
“Digital therapeutics are designed to close healthcare gaps by providing interventions when medical professionals cannot be there.”
Disease management programmes aim to couple the benefits of continuous data collection from drug delivery devices with structured, evidence-based treatment plans for common chronic conditions. Such programmes enable care teams to recommend interventions based on what the device data tells them, such as prescribing a different medication for hypertension if the data shows that the current one is not lowering blood pressure as intended. However, the first such programmes relied on in-person care, and those that did make use of technology often relied on proprietary systems that were disconnected from clinical software and largely unavailable to patients.
The Current Picture
Buoyed by rapid adoption of smartphones, the explosion of digital health applications over the past decade has put device data and disease management in the palms of patients’ hands. This has empowered patients to self-manage their health and facilitated communication with healthcare professionals, allowing patients to become more active participants in their own care. Unfortunately, the sheer volume of digital health applications, coupled with the lack of standards for vetting their clinical efficacy, has led to understandable scepticism among many in the medical community.
The latest evolution in the standard of healthcare – digital therapeutics – aims to address these issues (Table 1). As defined by the Digital Therapeutics Alliance, these products deliver medical interventions directly to patients. They are backed by evidence-based software that is subject to an evaluation process as rigorous as that applied to the approval of new drugs or medical devices through clinical trials.
| Patient Support Tool | Benefits | Drawbacks |
| Drug delivery devices | Enable self-administration | Analogue devices with no data to share |
| Connected devices | Data saved electronically | Data presented without context |
| Disease management | Evidence-based treatment plans | Largely in-person and proprietary |
| Digital health | Empower self-management | Many choices and no vetting process |
| Digital therapeutics | Brings approved medical interventions direct to patients | Limited adoption to date |
Table 1: Benefits and drawbacks of patient support tools.
Digital therapeutics are designed to close healthcare gaps by providing interventions when medical professionals cannot be there. This increases patient access to proven therapies, allows clinical staff to provide care to more patients in less time, enables clear alignment of treatment plans and patient care goals, and makes it possible for patients to receive care in their native language.
THE VALUE OF BRINGING TOGETHER DIGITAL, DEVICES AND SERVICES
The evolution of drug delivery illustrates how digital products are positioned to boost the standard of healthcare. It is worth noting, however, that digital health solutions and digital therapeutics are just one piece of the puzzle. Devices play an important role – specifically modern drug delivery devices that work with therapeutics by helping patients administer the proper dose of treatments for common chronic conditions. There are even specialised training devices that can help familiarise patients with how to use injectables, sprays or eye drops so they are confident once they have their actual therapies in hand.
Services, meanwhile, assist pharmaceutical companies with the design, development, formulation and testing of therapeutics. Analysis is a critical service for pharmaceutical companies to ensure that products adhere to quality and regulatory standards, meet customer expectations and deliver the right dose to a patient the first time and every time.
Each of these three components is important on its own, but the true value of digital, devices and services is realised when they work in combination. This is the theme in Aptar Pharma’s growth strategy (Figure 2) – most recently complemented by the acquisition of Voluntis and reflected in previous acquisitions ranging from Nanopharm and NextBreath to Noble and Cohero Health.
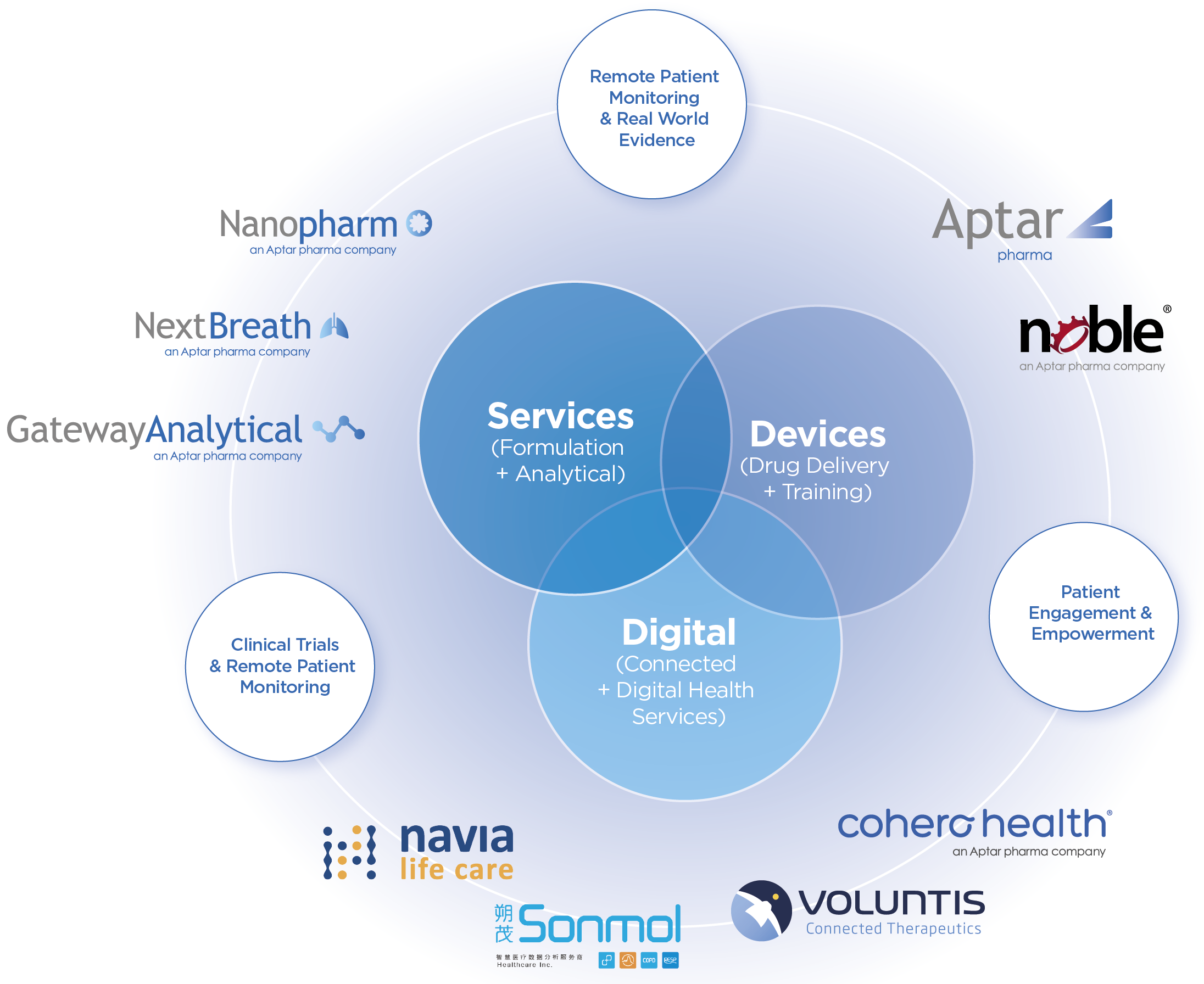
Figure 2: The long-term strategy of digital, devices and services.
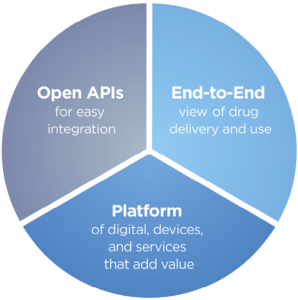
Figure 3: The benefits of an open, end-to-end platform API.
“Each of these three components is important on its own, but the true value of digital, devices and services is realised when they work in combination.”
THE BENEFITS OF HOSTING DIGITAL, DEVICES AND SERVICES ON AN OPEN, END-TO-END PLATFORM
As discussed, the new standard of healthcare depends on the ability of all healthcare stakeholders – provider, payer, pharmacy, pharma manufacturer and patient – to have access to the longitudinal data necessary for them to make informed healthcare decisions. This cannot be done if data remain in silos, regardless of who has created them, be it software vendors, device manufacturers or healthcare institutions.
The new standard of healthcare demands a new, unified experience for engaging with digital, devices and services. Aptar Pharma believes that this can only be done through the adoption of an open, end-to-end platform that paints a more complete picture of drug delivery and use for the entire healthcare ecosystem. There are three key phrases in the description of Aptar’s vision, “open”, “end-to-end” and “platform” (Figure 3). Let’s unpack what each one means and see how, together, they offer a level of insight into the use of therapeutics that has not been possible before.
Open
Healthcare has had walled gardens for too long. Leveraging open application programming interfaces makes it possible to connect digital, devices and services without writing custom integrations. Any healthcare stakeholder with value to add, whether it is a diagnostic device, digital therapeutic, data aggregator or clinical application, should have the ability to connect and integrate with other solutions.
End-to-End
Today, key data about each stage of using a therapy resides with a different stakeholder. The manufacturer makes the therapeutic, the physician prescribes it, the pharmacy fills the prescription, the insurer pays for it, the patient takes it and the care team follows up to see how it is working. An end-to-end view is necessary to get a more complete picture of drug delivery and use – to identify what obstacles prevent patients from getting the therapy they need, from adhering to the prescribed dosing requirements to achieving the desired therapeutic outcome.
Platform
Drug delivery devices become even more powerful tools when it is possible to layer digital health applications and services on top of them, especially when these tools have been created by trusted third-party partners with expertise that the designer’s organisation lacks. For example, the manufacturer of an inhaler can add a sensor that measures whether a full dose was inhaled, if the angle of inhalation was correct or whether the inhaler was shaken appropriately prior to actuation.
The End-to-End Platform in Action
When an end-to-end platform is in place, patients and their care teams can finally realise the high standard of care that healthcare has sought for so long. Care teams can provide patients with personalised digital therapeutics backed by clinical evidence, as well as the latest in predictive analytics.
Voluntis – a digital therapeutics company recently acquired by Aptar Pharma – has received 14 regulatory approvals in North America and Canada, amassed 13 years’ worth of clinical trial data and managed deployments covering more than 100,000 patients. The company’s approach to delivering patient-centred care in three key clinical areas demonstrates the power of the end-to-end platform in action:
- Oncology: Helping patients self-manage symptoms related to cancer treatment through communication, shared decision-making and personalised real-time recommendations can improve quality of life while limiting exposure to harmful treatments.
- Diabetes: Automated insulin dose recommendations coupled with coaching messages let care teams monitor patients remotely while meeting payers’ requirements for reimbursable telemedicine services.
- Anticoagulation: Using a solution developed in collaboration with Roche Diagnostics (Basel, Switzerland), patients on anticoagulation therapies are connected to diagnostic testing facilities that monitor the ratio of the self-administered vitamin K antagonist treatment.
CONCLUSION
The evolution of the market for patient support tools closely mirrors the evolution of Aptar Pharma’s business. Through organic growth, as well as mergers and acquisitions, the company’s focus has transitioned from drug delivery devices to connected devices to disease management to digital health to digital therapeutics. At the same time, Aptar Pharma is building an open, end-to-end platform to host the devices, digital applications and services that make it possible to see the complete picture of drug delivery and use. Not only does this serve the needs of the company’s partners, it enables it to support the healthcare ecosystem in providing a new standard of personalised care backed by evidence-based digital interventions. For patients managing chronic conditions, this leads to better outcomes and a better quality of life.

