To Issue 155
Citation: Koerner J, Bates M, “Improving Medication Adherence and Clinical Outcomes Through Connected Drug Delivery Devices”. ONdrugDelivery, Issue 155 (Dec 2023), pp 16–20.
Joachim Koerner and Marcus Bates discuss the challenge that medication non-adherence presents to the healthcare sector, and the potential value of connected digital health solutions as a way of overcoming this challenge.
“Twenty years ago, a seminal report from the WHO found that average medication adherence rates for patients with chronic conditions were around just 50%.”
Medication non-adherence and its many complications have posed a significant challenge to healthcare and the life sciences for decades. However, because many factors contribute to non-adherence, which can vary significantly based on the conditions a patient is managing, there is no one-size-fits-all solution to the non-adherence problem.
That said, the growing field of connected drug delivery solutions highlights the potential of purpose-built products to support patients managing chronic health conditions. Through education, engagement, communication, evidence-based recommendations and more, these solutions can guide patients through taking their medications, tracking their side effects and living their everyday lives.
To achieve these results – and to help shift the needle away from reactive disease management towards preventive care – organisations must consider how patients will use connected drug delivery solutions in tandem with their therapies. This may require a new approach to solution development, one that begins when the therapeutic itself enters the early stages of development.
THE CHALLENGE OF MEDICATION NON-ADHERENCE
Twenty years ago, a seminal report from the WHO found that average medication adherence rates for patients with chronic conditions were around just 50%. These rates were significantly lower in developing countries and for certain conditions, particularly asthma and high blood pressure.1 Additional research has shown that adherence rates have increased in the years since, but remain at less than 60%.2 The American Medical Association considers patients non-adherent if they take less than 80% of their prescribed medications.3
While a multitude of factors contribute to non-adherence, they tend to fall into five general categories:
“Connected drug delivery solutions are designed to help patients take their treatments as effectively and efficiently as possible.”
- Individual patient motivation: There are many personal reasons that patients may choose not to take medication – denial of diagnosis, cognitive impairment, religious or cultural aversion, history of substance use, fear of side effects or preference to allow health to decline without treatment.
- Social determinants of health: Limited access to reliable and convenient care, including the means to travel to in-person appointments or participate in telehealth appointments, may make it difficult for patients to renew prescriptions or speak to healthcare providers.
- Insurance coverage: Cost is a common barrier to adherence. This is especially the case for biologics or other highly targeted therapies, as well as for patients taking medications to manage multiple chronic conditions.
- The condition being treated: If a chronic condition is asymptomatic, as is common with autoimmune diseases, patients may not realise that they need to continue taking their medication. Additionally, non-adherence rates are shown to be higher for patients with psychiatric conditions.2
- The treatment prescribed: Patients often skip treatments that are difficult to take, such as pills that are hard to swallow or injectables that require self-administration. It is also common for patients to skip, or stop altogether, treatments with negative side effects.
The consequences of poor medication adherence are significant. In the US alone, non-adherence has been linked to an estimated 125,000 preventable deaths and up to US$300 billion (£240 billion) in direct and indirect healthcare costs.4 Non-adherence also contributes to poor clinical outcomes, as patients are likely to see a condition worsen if they are unable to treat it with the medication they have been prescribed.
THE VALUE PROPOSITION FOR CONNECTED DRUG DELIVERY DEVICES
Given the diverse challenges associated with improving medication adherence, it comes as no surprise that there is growing interest across the healthcare ecosystem for digital tools that help patients not only take their medications but also manage their chronic conditions. Connected drug delivery solutions are designed to help patients take their treatments as effectively and efficiently as possible (Figure 1).
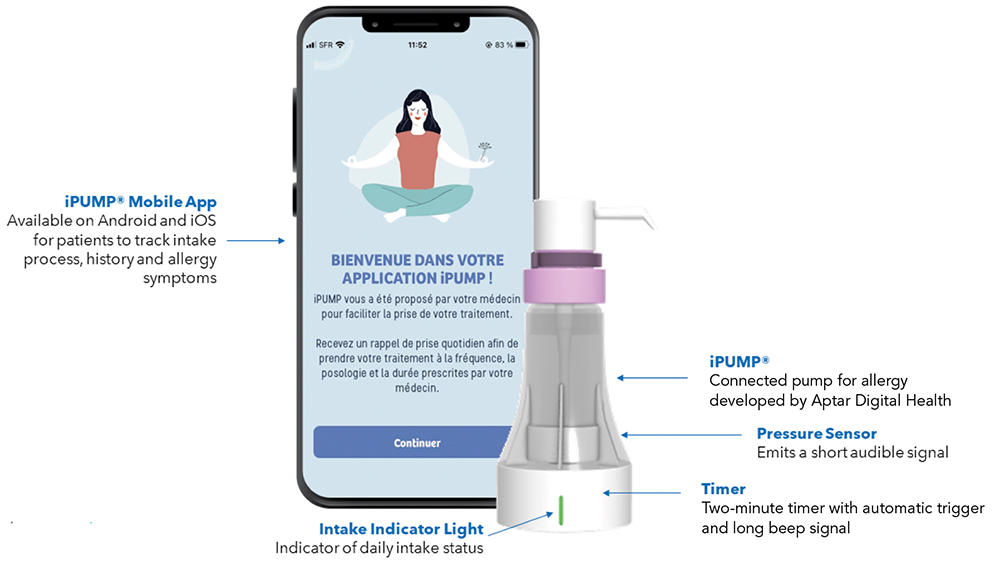
Figure 1: iPUMP®, the first connected allergy assistant developed by Aptar Digital Health and recently launched in France by Stallergenes Greer (Baar, Switzerland).
“As part of their goal of improving medication adherence and enhance chronic condition management beyond the clinical setting, there are 10 main ways that connected drug delivery solutions support patients.”
Some connected solutions use sensors to gather vital signs or other important information, whereas others rely on patient-reported outcomes (PROs), such as symptoms or side effects. Instructions for administration are also a common feature. From there, they aggregate and analyse data for multiple use cases, such as providing next-best action recommendations to patients, offering additional educational materials, assessing patient progress over the course of their treatment and providing updates to clinical care teams.
These solutions empower patients in three important ways. The first is providing them with a better understanding of their condition, as well as the importance of their therapy as part of their overall condition management plan. The second is a more personalised approach to treatment, as recommendations are based on their own data coupled with evidence-based treatment pathways. The third is an ability to receive feedback and communicate with care teams far more frequently than in the past, when patients were often limited to in-person appointments with specialists a few times each year.
The market for connected drug delivery solutions is growing. Grand View Research (CA, US) estimated the global market at more than $4.8 billion in 2022 and projected the market would exceed $25 billion by the end of the decade.5 The industry’s effort to improve medication adherence is one key factor driving this growth. Another is the increased prevalence of asthma, diabetes and other chronic conditions that require lifelong monitoring, management and engagement from patients.
“Along with logging side effects, connected devices can provide insight into which side effects are normal and which may require medical attention.”
10 USE CASES FOR CONNECTED DRUG DELIVERY DEVICES
As part of their goal of improving medication adherence and enhance chronic condition management beyond the clinical setting, there are 10 main ways that connected drug delivery solutions support patients. Critically, these use cases support development, commercialisation and real world monitoring of therapeutics.
Decentralised Clinical Trials
Connected devices let patients participate in clinical trials without the need for frequent in-person visits to the trial site. Trial sponsors can enrol patients from traditionally under-represented patient populations and geographies, giving them additional evidence of how a therapy works in practice.
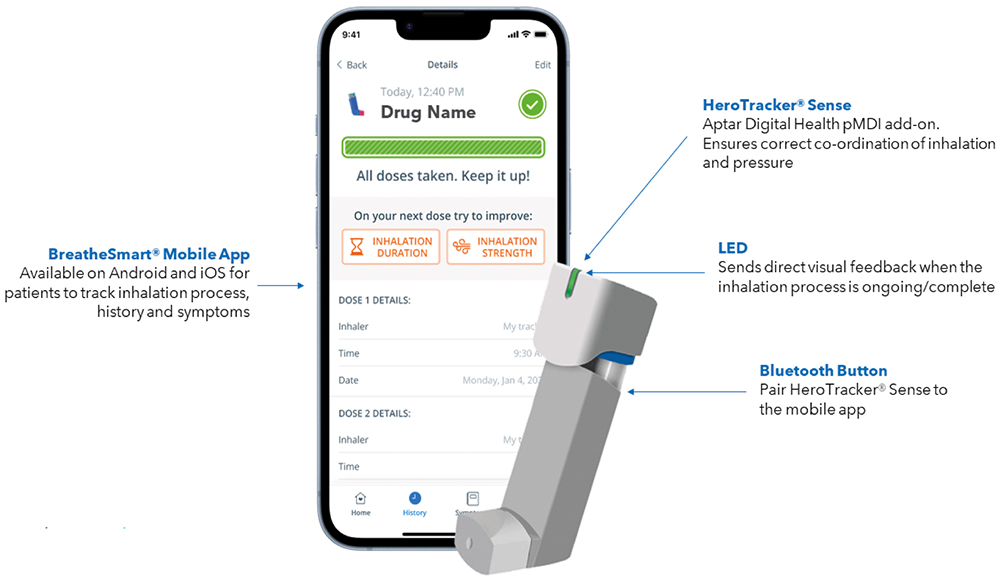
Figure 2: HeroTracker® Sense and BreatheSmart®, Aptar Digital Health’s digital solution for respiratory conditions.
Supporting Self-Administration
Tutorials can remind patients to shake an inhaler prior to actuation to get the correct dosage (Figure 2). They can also show patients the proper angle and demonstrate the correct pressure for injectables, which is a critical consideration for therapies that are administered on an infrequent basis and/or come with a high out-of-pocket cost (Figure 3).

Figure 3: AdhereIT®, Aptar Digital Health’s autoinjector add-on.
Providing Education
Patients can learn how a treatment works in their body, along with why it is important to take it even if they do not present symptoms. For certain conditions, patients can learn to identify which symptoms should prompt administration of a treatment and, in doing so, potentially prevent an acute care episode.
Meaningfully Communicating PROs
Instead of writing symptoms in a physical notebook or note-taking app, connected devices let patients log PROs as structured data and, if they choose, send that information to their clinical care team. These curated summaries keep healthcare providers informed of a patient’s condition without the need for a thorough review of their records.
Managing Side Effects
Along with logging side effects, connected devices can provide insight into which side effects are normal and which may require medical attention. Evidence-based, nonclinical recommendations for managing discomfort may help as well, and they can reduce the volume of non-urgent communication with a clinical care team.
A Platform for Supplemental Products
Giving patients a place to access their prescriptions, as well as other products approved by their physicians, from blood pressure cuffs to dietary supplements to diagnostic tests, provides a more integrated care experience and makes it easier for patients to obtain the products they need to manage their health and wellness.
Patient Support Programmes
Whether patients manage common chronic conditions or rare diseases, they benefit from connecting to others who can provide guidance and support. This is especially true for aspects of everyday life that are often not covered in conversations with their care team.
Motivation and Encouragement
Especially with life-long chronic conditions, patients face setbacks and have bad days. Providing encouragement tailored to a patient’s specific treatment plan and condition can help get them back on track.
Recommendations for Preventive Care
Connected devices can help determine the right course of action based on a patient’s current symptoms or predicted future risk through features such as screening questionnaires and virtual care triage tools. This enables care teams to provide preventive services instead of waiting for a patient to be admitted to hospital.
A Single Platform for Data Access
Market-leading connected devices sync to single, open platforms where, with their consent, patients can make data available to healthcare providers, insurers and life science organisations. This gives all stakeholders a longitudinal view of a patient’s progress towards clinical goals and metrics associated with outcomes-based arrangements they may be enrolled in.
“The payoff is that a solution goes through the same rigorous development and testing process as the therapeutic it will support.”
ENSURING THAT SOLUTIONS MEET PATIENTS’ NEEDS
For all their benefits, getting patients to consistently use connected drug delivery solutions and other digital health products remains an uphill battle. Only 40% of patients use the portals connected to their electronic health record systems6 and an estimated 70% of patients abandon remote monitoring devices and other assistive technologies.7 Numerous factors contribute to this disinterest, including, but not limited to, difficult set-up, low quality feedback, poor usability, low reliability and unnecessary features.8
Making sure that connected drug delivery solutions can meet the diverse needs of patients across a multitude of use cases will require an iterative approach to design, development and commercialisation. While this process may vary from one organisation to the next, there are generally six steps involved:
- Identify patients’ barriers to managing their condition and taking their therapeutic as prescribed
- Look holistically at patients’ needs and determine the user experience elements and solution workflows that can address them
- Create a solution prototype for stakeholders, including patients, to react to
- Incorporate feedback and make necessary adjustments before beginning full-scale development
- Ensure that solution development is tightly aligned with clinical development of the corresponding therapeutic
- Approach solution development and approval like a clinical trial, conducting summative studies and human factors studies; address all problems before the next phase of development begins.
Approaching the development of a connected drug delivery solution in this manner requires a significant up-front investment in time, energy and resources. It is also in stark contrast to the typical process of creating a standalone digital health application, especially one not regulated by authorised bodies.
The payoff is that a solution goes through the same rigorous development and testing process as the therapeutic it will support. As a result, the therapeutic and the solution are ready to go to market at the same time, helping to ensure that patients can get the support they need as soon as they begin a new treatment plan.
LOOKING TO THE FUTURE OF CONNECTED DRUG DELIVERY DEVICES
As valuable as today’s use cases for connected drug delivery solutions are, it is exciting to think about what the future may hold. For example, data aggregated onto a single platform makes it possible for industry stakeholders to better understand how individual therapies work across a patient population. This could allow healthcare providers to modify and improve treatment pathways, help payers determine which therapies have the greatest impact on clinical and financial outcomes and empower life science organisations to identify additional indications or other new development opportunities.
Additionally, connected solutions will further enable the industry to push preventive care upstream. Real-time insight into how patients experience symptoms and respond to therapies will allow for more informed and evidence-based decision support. The potential to provide recommendations for new treatments, including over-the-counter products or digital health solutions, is poised to change the way healthcare providers approach chronic condition management – a positive outcome that all healthcare stakeholders can agree on.
REFERENCES
- “Failure to take prescribed medicine for chronic diseases is a massive, world-wide problem”. WHO, Jul 2003.
- Foley L et al, “Prevalence and predictors of medication nonadherence among people living with multi-morbidity: a systematic review and meta-analysis”. BMJ Open, 2021, Vol 11(9), Article e044987.
- Brown M, Sinsky CA, “Medication Adherence: Improve Patient Outcomes and Reduce Costs”. AMA STEPS Forward, Jun 2015.
- Benjamin RM, “Medication Adherence: Helping Patients Take Their Medicines As Directed”. Public Health Rep, 2012, Vol 127(1), pp 2–3.
- “Connected Drug Delivery Devices Market Size, Share & Trends Analysis Report By Product, By Route Of Administration (Parenteral, Inhalational), By Application (Asthma, COPD, Diabetes Management, Others), By Region, And Segment Forecasts, 2023–2030”. Market Report, Grand View Research, 2023.
- Johnson C, Richwine C, Patel V, “Individuals’ Access and Use of Patient Portals and Smartphone Health Apps, 2020”. ONC Data Brief No 57, Sep 2021.
- Howard J et al, “Exploring the barriers to using assistive technology for individuals with chronic conditions: a meta-synthesis review”. Disabil Rehabil Assist Technol, 2022, Vol 17(4), pp 390–408.
- Park JI et al, “Lack of Acceptance of Digital Healthcare in the Medical Market: Addressing Old Problems Raised by Various Clinical Professionals and Developing Possible Solutions”. J Korean Med Sci, 2021, Vol 36(37), Article e253.

