To Issue 134
Citation: Edalat P, Hatamian M, “Smart Drug Delivery Devices Improve Medication Adherence: Here’s How”. ONdrugDelivery, Issue 134 (Jun 2022), pp 14–16.
Paul Edalat and Mehdi Hatamian take an in-depth look at medication non-adherence and how technology can be used to improve compliance rates and optimise patient outcomes.
Prescription medication non-adherence is a significant concern for medical providers as it can negatively affect patient outcomes and accounts for a notable portion of treatment failures, deaths and hospitalisations every year. Yet, despite the recognition this issue receives, it is estimated that nearly half of patients do not take their medications as prescribed.1
“A smart drug delivery device that collects patient usage data, such as dosage and timing, and shares it with the physician can improve medication adherence.”
WHAT IS MEDICATION ADHERENCE AND WHY IS IT IMPORTANT?
Medication adherence refers to how well a patient takes their medication as prescribed, meaning taking the correct dose correctly, at the right time and frequency. Adherence plays a crucial role in patient outcomes, including patients managing both acute and chronic conditions. Failure to adhere to medication instructions when trying to control any condition can worsen or progress the state of disease, prolong hospitalisations and adversely impact a person’s overall quality, and even length, of life.
Non-adherence can also increase the cost of care. According to a 2018 study, non-optimised therapies cost the US an estimated US$528.4 billion (£421.4 billion) in 2016, placing a significant burden on an already strained healthcare system.2
IDENTIFYING NON-ADHERENCE
A patient is considered non-adherent if they take their medication according to their provider’s instructions less than 80% of the time. The three main types of non-adherence include:
- Primary non-adherence – when the patient does not fill the prescription after their physician writes the order
- Non-persistence – when a patient stops taking their medication without their physician’s consent
- Nonconforming – when a patient does not take their medication as prescribed. This type of non-adherence includes skipping doses, taking medicines at incorrect times and taking more or less than prescribed.3
“If the patient is adhering to their regimen, the doctor can make appropriate adjustments, such as modifying the dose, changing the dose frequency or selecting a different drug altogether.”
CURRENT METHODS TO MONITOR ADHERENCE
Currently, several direct and indirect methods are used to measure medication adherence. Direct methods include direct observation or taking measurements of drug or metabolite concentration in body fluids. While direct methods are the most accurate, they are expensive and can be burdensome.
Patient self-reports are the simplest tool for measuring adherence. Other indirect methods include patient questionnaires, pill counts, prescription refill rates, patient clinical response assessments and diaries. These techniques are often inaccurate, as there is significant room for error, and patients often overestimate their own adherence.4
USING SMART TECHNOLOGY TO IMPROVE MEDICATION ADHERENCE
It can be challenging to track and monitor medication adherence. Without an accurate measurement of compliance, it can be difficult to evaluate the efficacy of a treatment plan, especially if an issue arises and a provider is unable to tell if a medication is not working or needs to be adjusted because the patient is not adhering to their regimen.
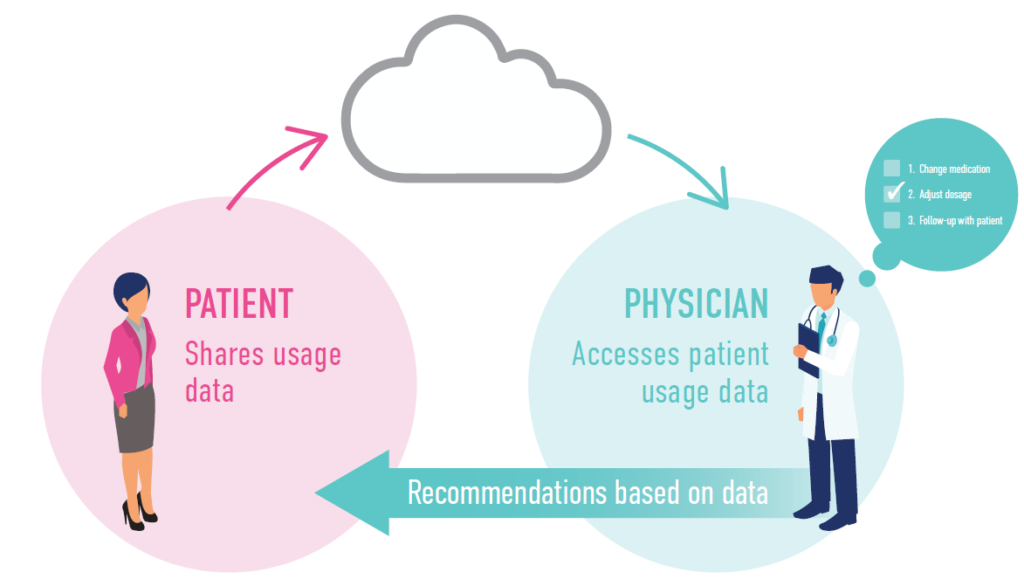
Figure 1: The patient uses the smart dosing device and the usage data is transmitted to a centralised database. The doctor can monitor and assess the patient usage data to make recommendations or adjustments to the patient’s treatment plan.
A smart drug delivery device that collects patient usage data, such as dosage and timing, and shares it with the physician can improve medication adherence. Such a device can allow physicians to track and monitor how well their patients are sticking to their prescribed medication regimen in real time, which can offer several benefits (Figure 1):
- Better-Informed Decision Making
Physicians will have accurate data to analyse how well a patient follows their medication schedule. This information will enable the physician to adjust a patient’s treatment plan based on their actual behaviour instead of their reported behaviour. If the patient is adhering to their regimen, the doctor can make appropriate adjustments, such as modifying the dose, changing the dose frequency or selecting a different drug altogether. These changes will be ineffective if a person is not sticking to their instructions in the first place. - Identify Underlying Reasons for Non-adherence
Accurate data can allow physicians to discover trends, which can then enable the physician to ask better questions about why a patient is not adhering to their medication regimen. For example, a patient prescribed to take medication twice a day may consistently take their medication as prescribed at night but not in the morning. The physician may uncover that the medication makes the patient sleepy or drowsy and may be able to adjust the dosage or prescribe a different medication altogether. - More Productive Follow-up
Appointments In addition to making adjustments to the patient’s treatment plan, physicians can also use the data from prescription delivery devices to have more productive follow-up appointments. Common reasons for non-adherence include forgetting to take doses, high drug prices, limited access to a pharmacy, the fear of or unreported side effects and the patient questioning if their medication is even necessary.
By identifying issues related to an individual patient’s adherence, physicians can have better conversations with them. The physician can help implement a programme or provide a smart device to help patients who forget to take medications on time. If a patient’s insurance doesn’t cover a drug, they can find a similar or generic drug that is covered under their plan. Physicians can also help patients understand the necessity of their medication and the consequences of not taking it.
“Monitoring adherence to opioid medications has unique challenges because these medications are more likely to be hoarded, diverted or sold than, for example, medications for blood pressure management.”
SPECIAL ATTENTION TO OPIOID NON-ADHERENCE
There is an elevated risk of overuse when considering potentially addictive medications, such as opioids. A patient’s side effects from overusing opioids include excessive sedation and respiratory depression. The rapid development of tolerance is also a significant concern, as it can increase the likelihood of addiction – a chronic disease characterised by compulsive drug-seeking behaviour despite any adverse effects.
According to the results from a prospective evaluation, the implementation of adherence monitoring can reduce opioid abuse by as much as 5%.5 However, monitoring adherence to opioid medications has unique challenges because these medications are more likely to be hoarded, diverted or sold than, for example, medications for blood pressure management.6
Using technology to connect the medication delivery device to the physician can alert the physician as soon as a pattern of misuse is detected. Additional technological advances, such as dose-controlled delivery, medication reminders and the ability to programme usage instructions into the device and only allow the prescribed dosage amount to be accessed according to the provider’s orders, can make it easier for patients to comply with their medication regimen.
THE NEED FOR IMPROVED SOLUTIONS
How well a patient adheres to their medication regimen is directly correlated to the overall efficacy of a treatment plan – patients who take their medications as prescribed have better results than those who do not. Given that many patients do not adhere to their medication regimens, the need for smart drug delivery systems to improve patient adherence is evident.
REFERENCES
- Brown MT, Bussell JK, “Medication adherence: WHO cares?”. Mayo Clin Proc, 2011, Vol 86(4), pp 304–314.
- Watanabe JH, McInnis T, Hirsch JD, “Cost of Prescription Drug-Related Morbidity and Mortality”. Ann Pharmacother, 2018, Vol 52(9), pp 829–837.
- Jimmy B, Jose J, “Patient Medication Adherence: Measures in Daily Practice”. Oman Med J, 2011, Vol 26(3), pp 155–159.
- Anghel LA, Farcas AM, Oprean RN, “An Overview of The Common Methods Used to Measure Treatment Adherence”. Med Pharm Rep, 2019, Vol 92(2), pp 117–122.
- Manchikanti L et al, “Does Adherence Monitoring Reduce Controlled Substance Abuse in Chronic Pain Patients?”. Pain Physician, 2006, Vol 9(1), pp 57–60.
- Fishman SM et al, “Adherence Monitoring and Drug Surveillance in Chronic Opioid Therapy”. J Pain Symptom Manage, 2000, Vol 20(4), pp 293–307.
Previous article
PUTTING PROCESS ENGINEERING INTO ACTIONNext article
SUPPORTING PATIENTS ON THE ROAD TO SELF-CARE
