To Issue 174
Citation: Wojcik J, Schochat L, “Integrating Digital Health Systems into Medical Device Ecosystems: Considerations and Strategies”. ONdrugDelivery, Issue 174 (Jun 2025), pp 6–10.
Jerzy Wojcik and Liat Shochat take a look at how digital health technologies are transforming the pharmaceutical and combination product sectors. They consider the challenges in bringing these technologies to market and how the full potential of connected health technologies can be achieved.
“FOR COMPANIES DEVELOPING DRUG-DEVICE COMBINATION PRODUCTS, SUCH AS AUTOINJECTORS, INHALERS, INFUSION SYSTEMS AND PFSs, THE QUESTION IS NO LONGER WHETHER CONNECTIVITY WILL BE REQUIRED BUT WHEN AND HOW TO INTEGRATE IT EFFECTIVELY.”
As advancements in healthcare continue to evolve, so too must the products and systems that support them. For companies developing drug-device combination products, such as autoinjectors, inhalers, infusion systems and prefilled syringes (PFSs), the question is no longer whether connectivity will be required but when and how to integrate it effectively. Successful integration requires a holistic approach that spans stakeholder alignment, design innovation, development rigour and strategic business transformation.
Connected combination products are the next frontier in value-added medicine. These digitally enabled devices do more than just deliver therapies – they provide real-time insights into patient behaviour and wellbeing, enable proactive clinical intervention and create new opportunities for differentiation in a competitive marketplace. Integrated sensors and communication modules can track dosing events, monitor device usage and adherence patterns and feed data to cloud-based platforms that can support clinical decision making, pharmacovigilance and population health analytics. This convergence is enabling a shift from episodic treatment to continuous, personalised care.
“SUCCESS DEMANDS A STRATEGIC, CROSS-FUNCTIONAL APPROACH THAT NOT ONLY INTEGRATES THESE ELEMENTS BUT ALSO ALIGNS PRODUCT DEVELOPMENT WITH REGULATORY EXPECTATIONS IN A DYNAMIC LANDSCAPE.”
However, bringing these technologies to market is inherently complex, requiring careful considerations across four key domains – stakeholder needs, device design, development programmes and business strategy (Figure 1). Success demands a strategic, cross-functional approach that not only integrates these elements but also aligns product development with regulatory expectations in a dynamic landscape – including the US FDA’s evolving approach to software as a medical device and the EU Medical Devices Regulation (MDR)/In Vitro Diagnostic Medical Devices Regulation (IVDR) requirements for software and general safety and performance, as well as the classification implications for connected systems.

Figure 1: Key considerations and inputs into developing a connected combination product.
STAKEHOLDER CONSIDERATIONS
Connected combination products sit within a complex ecosystem of stakeholders whose perspectives and needs are central to success. These include:
- Patients, who seek intuitive, reliable and discreet devices that deliver meaningful insights while ensuring privacy and security
- Healthcare providers, who require actionable, accurate and timely data that integrates seamlessly into clinical workflows
- Caregivers, who benefit from tools that provide support, guidance and monitoring capabilities for those they assist
- Regulatory authorities, who demand robust evidence of safety, effectiveness, performance and cyber security compliance
- Payers and healthcare systems, who evaluate the economic impact and clinical value of connected solutions
- Internal stakeholders, such as R&D, quality, regulatory affairs, marketing and executive leadership, who drive development priorities, ensure compliance and guide strategic direction.
Each of these groups define “value” and “risk” differently. Patients value usability, privacy and support in managing their condition. Providers prioritise clinical utility and workflow integration. Regulators focus on compliance and public safety. Payers evaluate cost-effectiveness and outcomes. Internal teams may focus on time-to-market, resource allocation and long-term competitiveness.
Stakeholder needs must be considered from the earliest stages of product planning. Their input informs design, risk management and commercial strategy. Failure to involve all stakeholders early can lead to significant consequences: delayed approvals, product redesigns, low adoption rates, negative user experiences and reputational harm.
A holistic stakeholder engagement strategy ensures that development efforts are aligned with real-world needs, thereby reducing rework, improving usability and increasing the likelihood of successful adoption and sustained market presence.
DESIGN CONSIDERATIONS
Designing connected devices fundamentally differs from designing traditional standalone systems in several ways. Traditional systems typically focus on mechanical performance and drug delivery functionality. Connected systems, by contrast, require integration of software, wireless communication, data management and cyber security into a cohesive platform. This expands the scope of design to include usability under dynamic conditions, additional data integrity, cloud-based data exchange and interoperability with digital health infrastructure.
Connectivity must be a core design element, not an afterthought. Adding connectivity to an already designed device often results in misaligned components, user dissatisfaction and regulatory delays. A holistic, end-to-end design approach is essential to ensure that each element – from hardware architecture to user interface – is optimised for interoperability, usability, safety and performance (Figure 2).
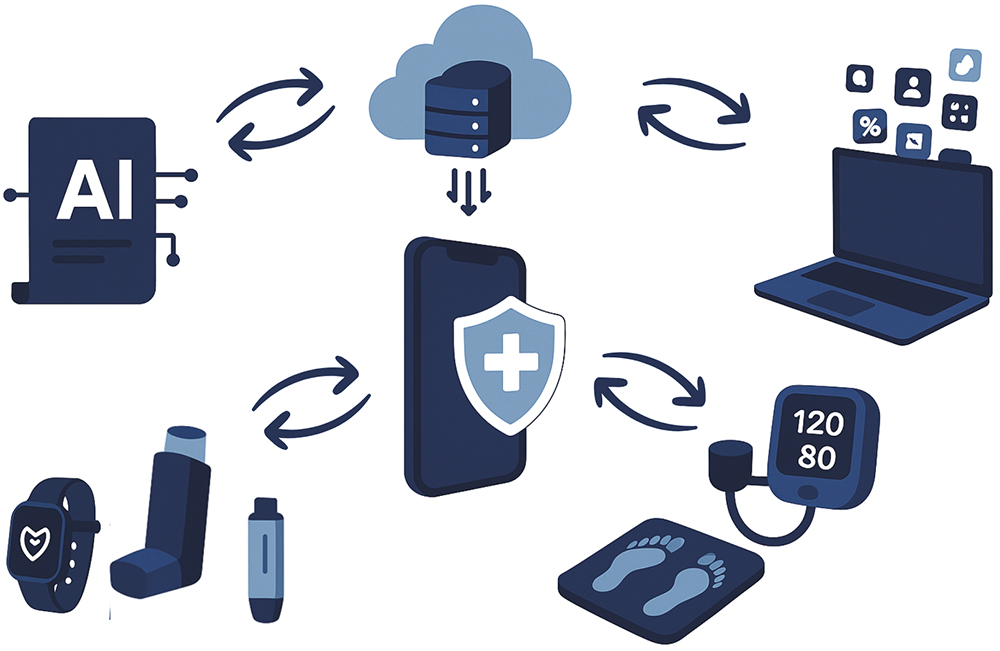
Figure 2: Generic system architecture overview showing the interactions between subsystems.
However, intentional retrofitting of legacy systems – particularly when the base product is well-established and clinically proven – can be a strategic path forward. In these cases, design considerations must focus on carefully preserving the core functionality and regulatory approvals of the legacy device while thoughtfully integrating digital components. Success with this approach requires a disciplined risk assessment to evaluate the impact of new components on device and drug stability, usability and user interface design. Custom enclosures, modular add-ons or external smart accessories may be employed to introduce connectivity with minimal disruption. Human factors testing and re-validation of drug-device interactions are essential to mitigate the risks associated with retrofit solutions and to ensure compliance with current standards.
Key Design Aspects
- Human Factors: Connected devices alter user interaction. Interfaces must support a range of abilities, environments and experiences with minimal cognitive load. IEC 62366-1 usability validation ensures devices are both safe and user-friendly.
- Cyber Security: Connected devices are susceptible to evolving digital threats. Security must be embedded from the outset using standards such as ISO/IEC 27001 and FDA guidance. Inadequate planning can result in data breaches or device manipulation.
- Power Management: Wireless communication and onboard computing increase energy demands. Trade-offs must balance battery life, device size and user expectations.
- Interoperability: Systems must be able to seamlessly exchange data with health IT platforms. HL7 fast healthcare interoperability resources (FHIR) compliance, harmonised data formats and reliable data synchronisation are foundational considerations.
- Compatibility with Drug Product: Thermal or mechanical impact of sensors, wireless modules and other electronics may affect the drug’s stability. These impacts require re-evaluation of stability studies and extractables/ leachables profiles.
Design missteps can lead to severe downstream consequences. Failure to address human factors may result in user errors that can compromise therapy adherence. Inadequate cyber security exposes patient data and brand reputation. Poor interoperability hinders clinical workflow integration and delays adoption. Each of these factors underscores the need for rigorous, multidisciplinary design planning from project inception.
DEVELOPMENT PROGRAMME CONSIDERATIONS
Adopting the right development approach is critical for connected systems. These products demand a level of integration and complexity that surpasses traditional device development. A systems engineering framework can provide the structure to harmonise functional requirements, technical specifications, risk controls and regulatory demands while still integrating into the drug development programme as a combination product. It facilitates traceability, accountability and iterative validation across the product lifecycle.
Without a systems engineering approach, teams risk misalignment between hardware and software, leading to rework, delays and potential compliance failures. Fragmentation often results when teams are assembled ad hoc or operate in silos, causing communication gaps, inconsistent documentation and missed dependencies across subsystems.
Cross-functional collaboration is essential from the start. Effective development programmes integrate engineering, clinical, quality, regulatory, cyber security and commercial stakeholders in a co-ordinated and continuous manner. This multidisciplinary engagement allows organisations to foresee and address critical challenges early.
Defining the development scope early is equally vital. It sets the foundation for resource planning, partner selection, budgeting and timeline management. Programmes that delay scope definition often face cascading issues – unclear requirements, missed regulatory expectations, unanticipated testing needs and friction between technical and commercial teams.
Best Practices
- Cross-Functional Teams: Embed a collaborative culture by involving key disciplines from planning through execution.
- Systems Engineering: Use structured methodologies to ensure alignment of system functions and quality requirements.
- Risk Management: Use ISO 14971 and ISO 60812 principles to proactively identify, assess and mitigate risks to safety and quality – including those related to cyber security and interoperability.
- Early Scope Planning: Clarify goals, constraints and success criteria early to guide the entire development process.
“CONNECTIVITY AFFECTS BUSINESS MODELS, OPERATIONS AND COMMERCIALISATION STRATEGIES.”
BUSINESS CONSIDERATIONS
Connectivity affects business models, operations and commercialisation strategies.
Key Business Shifts
- Organisational Capabilities: Companies must develop new competencies in data governance, cyber security operations, cloud platform management, software validation and post-market surveillance. Supporting digital operations requires establishing a robust infrastructure for firmware updates, managing back-end systems and addressing ongoing customer support for digital products.
- Demonstrating Value: Demonstrating value to stakeholders requires targeted messaging. For patients, this means clearly showing how the device enhances quality of life, improves adherence or offers actionable health insights. For providers, value may lie in workflow integration and better clinical outcomes. Payers look for cost-effectiveness, reduced hospital visits and data that support reimbursement models. Health economic evaluations, user feedback and real-world evidence are essential in building a strong value proposition.
- Strategic Partnerships: Partnerships with cloud infrastructure providers, cyber security experts, software developers and digital health startups can accelerate development, reduce technical complexity and ensure compliance. Collaboration with healthcare institutions and patient advocacy groups can also strengthen clinical relevance and user engagement.
- Lifecycle Management: Even more than traditional devices, connected products require continuous lifecycle oversight. Software updates must be planned, validated and deployed securely. Cyber security threats must be monitored and mitigated through real-time surveillance. Changes to companion apps or back-end systems must maintain regulatory compliance, interoperability and data integrity. Lifecycle management becomes an active, iterative process that demands co-ordination across technical, regulatory and customer-facing teams.
Executives and technical leaders must recognise that connected product development is more than a one-time investment – it is a commitment to long-term digital operations. Organisations must evaluate their readiness, not only to build these products but to support them post-launch. This shift impacts budgeting, staffing and strategic planning. Traditional go-to-market frameworks need to evolve to reflect the continuous nature of digital health engagement and regulation.
CONCLUSION
Connected devices are reshaping the future of care delivery. However, success demands more than technical innovation – it requires aligning stakeholder needs, designing holistically, executing robust development programmes and evolving business strategies.
As leaders reflect on their connected product initiatives, they must ask:
- “Do I fully understand the complexity of connected product development, and where the major risks and blind spots exist?”
- “What qualities and expertise should I look for in a development partner who can support both the technical and regulatory demands of a connected device?”
- “How do I evaluate whether a partner can align with my business strategy and manage cross-functional integration effectively?”
- “Who within my organisation should be leading these conversations, and who should we engage with externally to ensure a comprehensive strategy?”
The ideal development partner should have a proven track record in regulated digital health product development, a deep understanding of global regulatory frameworks and the ability to operate across the software, hardware-mechanical interface, human factors and cyber security domains. They must be capable of supporting collaborative workflows and offer a strategic vision that complements the company’s internal goals and infrastructure.
Internally, leadership should involve key members from R&D, regulatory affairs, clinical, quality, IT, marketing and business development. These teams must work together to form a unified vision and execution plan. Externally, companies should engage not only with technology vendors and regulatory consultants but also with clinical partners, patient groups and healthcare systems to ensure the product delivers tangible value across the healthcare ecosystem.
To conclude, connected products are not simply innovations, they are platforms that can transform how therapies are delivered and experienced. Choosing the right partner – one who can bridge technical, regulatory and strategic demands – is critical to unlocking the full potential of connected health technologies and delivering lasting impact.

