To Issue 180
Citation: Petersson G, “Expanding Opportunities for Inhaled Drug Delivery.” ONdrugDelivery, Issue 180 (Nov 2025), pp 74–78.
Dr Gunilla Petersson considers the challenges associated with efficiently delivering drugs to the lungs and the potential of nanoparticle-based formulations to achieve high lung deposition of small molecules and biologics, using gentle particle processing techniques that enable the delivery of sensitive drugs.
Whether to treat localised respiratory disease or because the lung provides a fast, non-invasive and efficient route of delivery for systemic effect, the administration of pharmaceuticals to the lung is gaining increased attention; even beyond treatments for globally prevalent diseases such as asthma and chronic obstructive pulmonary disease (COPD). Although well established and accepted, oral and parenteral administration of drugs can require much higher doses than topical administration to the lung, which can lead to significant unwanted systemic exposure and the resulting side effects. However, the lung also presents unique challenges due to the complex structure of the airways, the presence of various protective barriers and the need to generate a suitable aerosol using an inhaler.
Respiratory diseases represent one of the world’s biggest health concerns and are a leading cause of death worldwide.1 They include conditions such as COPD (which the World Health Organisation lists as the world’s third leading cause of death),2 pneumonia, asthma and lung cancers. Several rare lung diseases, such as pulmonary arterial hypertension and cystic fibrosis, are life -shortening and have a severe impact on quality of life. Idiopathic pulmonary fibrosis is deadly, and patients are given only a short life expectancy following a diagnosis.
Systemic delivery via the lung is often applied to obtain a fast onset of action. This is advantageous in treating the symptoms of neurological disorders such as Parkinson’s disease; can reduce feelings of agitation in bipolar disease and schizophrenia; and can help alleviate acute and breakthrough pain, for example, in cancer patients. For diabetics, inhaled insulin provides a less invasive alternative to frequent needle use.
The main advantage of delivering by inhalation directly to the lung to treat respiratory disease is that the actual site of action is targeted, allowing for localised treatment that minimises the required dose and any systemic side effects, with a tenfold higher lung dose reported for several drugs reformulated for lung delivery.3 A reduction in dose is particularly advantageous for delivering novel or very expensive biologics or gene therapy vehicles, which have dramatically changed the development landscape for research organisations focused on respiratory diseases.
LUNG DRUG DELIVERY SYSTEMS: A CHALLENGE FOR PULMONOLOGISTS & FORMULATORS
For an inhaled particle or droplet that contains a drug to reach a disease target in the lung, it must first negotiate the relatively narrow and bending regions of the mouth, throat and perhaps the upper airways to avoid unintended deposition there, before reaching the specific disease targets or receptor locations. The anatomical structure of the airway system is complex and is characterised by 23 generations of branching airways ending with the alveoli. Diseased airways may be constricted, collapsed, partially blocked by mucus or bacteria biofilms, or scarred and stiffened. All these abnormalities may inhibit efficient breathing and oxygen uptake by the patient.
Particles are mostly deposited in the lung by inertial impaction, sedimentation or diffusion. Inertial impaction tends to occur in the upper airways when particles’ velocity and mass cause them to collide into the airway walls. Sedimentation occurs more often in more peripheral airways, and is driven by gravity, so it can be influenced by breath-holding to allow gravity to have an effect. Diffusion occurs through Brownian motion and is relevant to particles of less than 1 μm in diameter.4,5 Thus, regional deposition in the throat or lungs is controlled mainly by the patient’s breathing patterns and particle size. To avoid losses and irritation in the throat and to maximise peripheral lung deposition, small particles combined with a low inhalation flow rate is recommended. Particles may, if deposited in the upper airways, provoke coughing during inhalation treatment,6 thus limiting drug penetration and causing the patient discomfort. Conversely, efficient powder dispersion from a dry powder inhaler (DPI) often requires a strong inhalation effort and an increased risk that particles will not pass further than the back of the mouth and the throat.
Interstitial lung diseases that lead to severe breathing difficulties and consistent coughing, such as pulmonary fibrosis, are located mainly in the distal alveolar region, which is reached via the smallest airways in the lung. Consequently, to access this region meaningfully, ultrafine particles are required in combination with a device that permits a slow breathing technique.7 This requires both highly dispersible powders in DPIs or a type of active liquid inhaler, usually a nebuliser. To minimise patient effort needed and treatment time, high drug load formulations are preferred, as these reduce the powder amount to inhale and the risk for coughing.
“MACROPHAGES INGEST AND DESTROY INVADING PATHOGENS, AS WELL AS DRUG PARTICLES IN THE 0.5–6 μm RANGE. CONSEQUENTLY, PARTICLES OF LESS THAN 500 nm ARE AN ADVANTAGE IN AVOIDING THIS FORM OF CLEARANCE.”
The physiological barriers of the lung are mainly mucociliary clearance, whereby cilia remove excess mucus, including any adhered drug particles not yet dissolved for absorption, and macrophageal clearance. Macrophages ingest and destroy invading pathogens, as well as drug particles in the 0.5–6.0 µm range. Consequently, particles of less than 500 nm are an advantage in avoiding this form of clearance.8 Three-dimensional biofilms generated by invading bacteria limit the access of antibiotics or other drugs that need contact with the lung epithelium. Bacteria may hide in the biofilm network with poor drug (antibiotic) access and, consequently, the infection becomes chronic through repeated flare-ups. This may also lead to antibiotic-resistant bacteria.
Many drugs will be quickly absorbed and cleared unless they are designed for extended residence time in the lung, which permits once or twice per day inhalations. One design strategy is to use poorly soluble drugs like the well-established inhaled glucocorticosteroids. However, it is a delicate balance to design drugs that have an optimal dissolution rate and lung retention, which is why formulators often need help balancing the in vivo drug concentration versus time profile (Figure 1).
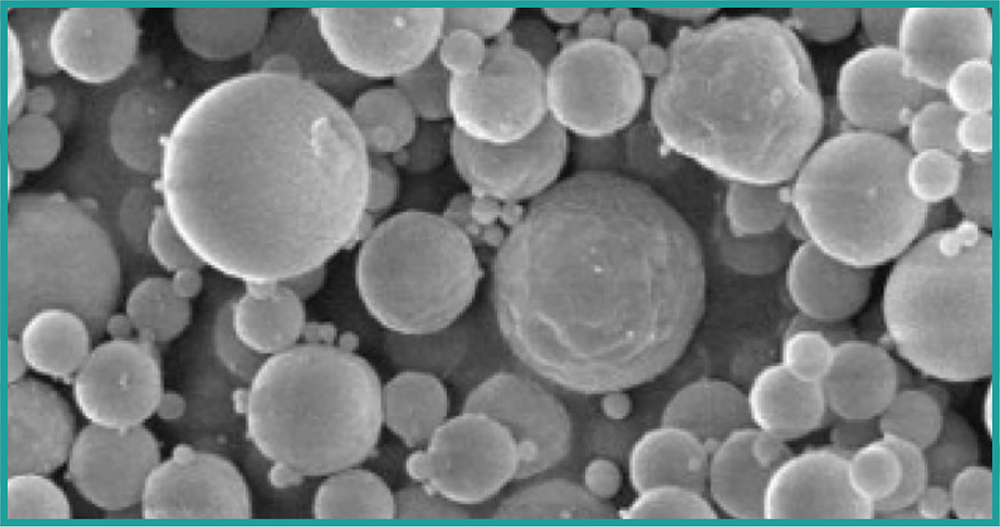
Figure 1: Direct manufacturing of particles suitable for inhalation.
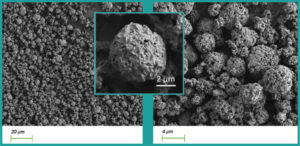
Figure 2: Nanoclusters of inhalable size.
Device and formulation interactions is another area of consideration for lung delivery. Any powder formulation will have to be of the relevant particle size for lung access, i.e. less than approximately 5 µm (Figure 2), which often makes powder “sticky” and prone to agglomerate and/or adhere to surfaces within the inhalation device. The patient’s inhalation force is used to disperse the powder during a short breath (1–3 seconds), which means that a certain minimum inhalation capacity is required to achieve efficient powder delivery. This is a concern for patients with severely diseased lungs, and sometimes liquid formulations delivered via nebulisers must be used instead.
Liquid inhalers do not offer a fast treatment time and, when poorly soluble drug particles held in a suspension are administered, a significant fraction of the drug will be retained in the device. The main reason for this retention is due to the small holes in the nozzle filtering out the particles. There is also a risk of clogging in the micron-sized nozzle holes. For some nebulisers, these phenomena lead to an even slower delivery rate using traditional micro-suspensions.
NANOFORMED API FORMULATIONS
The potential advantages of nanoformulations for effective delivery to the lung of small molecules and biologics are numerous and have been reflected in the literature. Firstly, nanoformulated drugs improve dissolution, solubility and bioavailability due to their smaller size and higher surface area:
- Poorly soluble drugs milled to nanoparticles avoid accumulation in the lung due to faster and complete dissolution9
- A nebulised glucocorticosteroid nanosuspension has a faster dissolution and absorption rate in the lung versus a microsuspension of the same drug10
- Mucociliary clearance of drug particles reduces the dissolved and bioactive fraction of poorly soluble drugs less for smaller particle sizes.11
Ensuring the dispersion of sticky, ultrafine (nano and sub-micron) particles enables inhalation of drugs, particularly for severely diseased lung patients:
- Efficient delivery of dry nanoparticles has been accomplished by spray-drying of nano-embedded microparticles (NEMs)12,13
- Nanoclustering of crystalline nanoparticles to porous particles of inhalable size reduces particle cohesion and increases the powder dispersibility for inhalation14,15
- Nanoclusters of submicron size may also be encapsulated in spray-dried matrices such as NEMs.
Nanoformulations allow for improvement of drug adhesion and penetration related to biofilms and mucus in infected lungs:
- Nanoparticles have been widely studied to overcome biofilms; however, their surface charge needs to be controlled to be positively charged15,16
- Nanoparticles have been found to have more efficient mucus penetration in the lung.17
Higher drug load in dry powders minimises the patient inhalation burden of repeated inhalations of high powder amounts, e.g. inhaling from five to ten capsules in sequence.
- Formation of nanoclusters for inhalation are highly dispersible with low amounts of excipients, even with just the pure drug.12
Reduced throat deposition and a higher lung dose by combining highly dispersible powders with low flow rates:
- A study comparing differently sized, inhaled particles indicates that cough reflexes could be avoided using smaller particles to reduce throat and upper airway deposition6
- In silico modelling and in vitro patient-simulated testing show a clear effect of particle size and inhalation flow rate on both throat and lung deposition.18
Finally, there is an increase of delivered dose output using liquid nebulisers:
- Delivery of budesonide as nanoparticles over microparticles increases the average dose (≤5 µm) two-fold19
- Control of drug particle shape – avoiding needle-shaped particles – is very important when using nebuliser delivery.20
“IT IS THE ONLY TECHNOLOGY CAPABLE OF MANUFACTURING NANOPARTICLES AT THE LOWER END OF THE NANO RANGE
WITHOUT SOLVENTS, EXCIPIENTS AND COMPLEX PRODUCTION PROCESSES.”
NANOFORM’S CAPABILITIES
Nanoform’s proprietary Nanoforming technology enables the production of small-molecule API nanoparticles without excipients and solvents. The manufacturing process is based on the precipitation of the API from a supercritical carbon dioxide (scCO2) solution, where precise process parameter control can lead to tight particle-size distribution and the desired crystalline or amorphous form. It is the only technology capable of manufacturing nanoparticles at the lower end of the nano range without solvents, excipients and complex production processes. Nanoparticles may be used in liquid suspensions or encapsulated into a spray-dried matrix for inhalation, either as individual nanoparticles or as submicron nanoclusters, e.g. to facilitate blending of different drugs in drug combinations or to tune drug dissolution rate.21
The Nanoforming process used for inhaled nanoparticles is compared to the use of conventional nanomilling in Table 1. The Nanoform Biologics platform addresses water soluble, sensitive drugs such as peptides, proteins and oligonucleotides. Traditionally, spray drying is attempted as the first formulation route for DPIs, but due to the demanding process – which involves heat to evaporate the solvent (water) immediately after droplet formation – as well as during secondary drying in the cyclone where particles are collected, some drugs do not tolerate spray drying. The platform uses nebulisation to form the droplets and dry gas at room temperature to remove the water phase, which is less stressful for sensitive drugs.
| Nanomilling (wet bead milling) | Nanoforming |
| Multiple process steps; bead milling, separation of beads and nanoparticles, potential need for recrystallisation of surfaces post milling. | One step, semi-continuous process forming dry, crystralline or amorphous nanopartices. |
| Higher energy, top-down process to break microsized crystals into nanosized with poor control of particle characteristics, potential amorphous surface material, risk of crystal defects. For very small particles, long milling times and cooling may be needed. Particles are re-circulated many times in the milling system. | Gentle, bottom-up process to improve control of particle size distrubution, shape and crystallinity/polymorph. Drug to be soluble in CO2 (predictive tool availability). No recirculation of particles during processing. |
| A complex process with many process parameters to adjust for each new API; bead material and size, rotation speed, time, drug media content, stabilisers (steric and/or electrostatic stabiliser), stabiliser content, mill movement pattern, temperature control, particle harvesting. | CO2 removed after formation of particles. No organic solvent used and potential to recycle CO2. |
| Liquid medium selected for bead milling should not dissolve the drug, to control and maintain particle size distribution during milling and storage. | Low amounts of surfactant needed to facilitate re-dispersion. |
| Significant amounts of polymers and/or surfactants (often two) to stabilise suspension during milling and storage. | Nanoforming process step as part of an aseptic process line. |
| For use in suspension formulations (injectable, inhalable, ophthalmological), need to sterilise the suspended particles. | For use in suspension formulations (injectable, inhalable, ophthalmological), need to sterilise the dry particles. An aspirational objective is sterilisation using scCO2. |
| Liquid intermediate (nanosuspension), chemical/physical stability may be challenging, risk for mircobial growth. | Dry intermediate (nanoparticles or nanoaggregates in bulk), chemical/physical stability likely less challenging, no microbial growth. |
Table 1: The Nanoforming process versus conventional nanomilling.
The platform process used for inhaled particles of standard excipients (including peptides and proteins) delivers material with similar characteristics as spray-dried material. These include a tight particle size distribution around a target of 2–3 µm, high dispersibility with fine particle fractions of up to 80% of the delivered dose and high drug loads in the range of 50–80% of the protein with a particle density suitable for efficient filling of standard capsules or blisters. Formation of protein aggregates was confirmed to be low using size exclusion chromatography, both post-processing and during storage.
Nanoform has experience in nanoforming and formulating APIs for lung delivery. Studies have seen the generation of particles for incorporation into clients’ formulations and include:
- Crystallisation of poorly soluble, difficult-to-crystallise drugs for inhaled delivery
- Nanosuspension, including nanoclusters, for nebulisation using a vibrating mesh inhaler
- Direct manufacturing of particles of peptides/proteins in the appropriate size range with optimal aerosolisation performance using the Nanoform Biologics platform.
REFERENCES
- “Sharing the WHO report on chronic respiratory disease: patient organisation toolkit”. European Lung Foundation, 2025.
- “The silent killer: why chronic respiratory disease deserves global attention”. WHO, 2024.
- “AR-501 (Panaecin™) Inhaled Gallium Citrate for Chronic Lung Infection in CF”. Company Webpage, Aridis Pharmaceuticals, accessed Sep 2025.
- Ariyananda PL, Clarke SW and Agnew JE, “Aerosol delivery systems for bronchial asthma”. Postgrad Med J, 1996, Vol 72(845), pp 151–156.
- Mortonen T and Yang Y, “Deposition mechanics of pharmaceutical particles in human airways” (Hickey AJ, ed). Marcel Decker, Inhalational Aerosols, 1996.
- Kanth PM, Alaienia C, Smaldone GC, “Nebulized mannitol, particle distribution, and cough in idiopathic pulmonary fibrosis”. Respiratory Care, 2018, Vol 63, pp 1407–1412.
- Phalen RF, Raabe OG, “The evolution of inhaled particle dose modeling: A review”. J Aer Sci, 2016, Vol 99, pp 7–13.
- Hague S et al, “Disposition and safety of inhaled biodegradable nanomedicines: Opportunities and Challenges”. Nanomedicine, 2016, Vol 12(6), pp 1703–1724.
- Hovdal IC et al, “Pharmaceutical compositions comprising nanoembedded microparticles and methods of use”. Patent WO2022023456A1.
- Kraft W et al, “The pharmacokinetics of nebulized nanocrystal budesonide suspension in healthy volunteers”. Department of Medicine Faculty Papers, 2004, paper 197.
- Usmani O, “Exploring Aerosol Absorption in Humans: Pharmacokinetics of Monodisperse Fluticasone Propionate”. RDD Conference Proceedings, 2014, pp 155–162.
- Party P et al, “Formulation and In Vitro and In Silico Characterization of ‘Nano-in-Micro’ Dry Powder Inhalers Containing Meloxicam”. Pharmaceutics, 2021, Vol 13(2), p 211.
- El-Gendy N et al, “Development of budesonide nanocluster dry powder aerosols: preformulation”. J Pharm Sci, 2012, Vol 101(9), pp 3434–3444.
- Baltezor MJ, Kuehl PJ, Ung K, “Aggregated High Surface Area Particle Technology for Pulmonary Drug Delivery”. RDD Conference Proceedings, 2020, Vol 2, pp 329–333.
- Zhao J et al, “Elucidating inhaled liposome surface charge on its interaction with biological barriers in the lung”. Eur J Pharm Biopharma, 2022, Vol 172, pp 101–111.
- Sahli C et al, “Recent advances in nanotechnology for eradicating bacterial biofilm”. Theranostics, 2022, Vol 12(5), pp 2383–2405.
- Alp G, Aydogan N, “Lipid-based mucus penetrating nanoparticles and their biophysical interactions with pulmonary mucus layer”. Eur J Pharm Biopharm, 2020, Vol 149, pp 45–57.
- Clark AR, “The Role of Inspiratory Pressures in Determining the Flow Rates Though Dry Powder Inhalers; A Review”. Curr Pharm Des, 2015, Vol 21(27), pp 3974–3983.
- Brun E et al, “Increasing the Lung Dose of Inhaled Suspensions – Comparison between Microsuspension and Nanosuspension Formulations Delivered by a Breath-actuated Mesh Nebuliser”. DDL conference, 2024.
- Vaghi A et al, “In vitro comparison of nebulised budesonide (Pulmicort Respules®) and beclomethasone dipropionate (Clenil® per Aerosol)”. Pulm Pharmacol Ther, 2005, Vol18(2), pp 151–153.
- Van Oort MM, Hong JN, “Aggregate particles comprising nanoparticulate drug particles”. Patent EP2836204 B1, 2015.

