To Issue 158
Citation: “Interview: Sandy Munro, Vectura”. ONdrugDelivery, Issue 158 (Apr 2024), pp 30–34.
Q Please could you give us an overview of Vectura as a company, its industry offering, and your role in the organisation?
A Today, Vectura is a CDMO specialising in inhaled product development, offering those services to other companies across various inhalation technology platforms. We can help customers develop DPIs, nebuliser products – including those using handheld vibrating-mesh devices – pMDIs and also intranasal products.
We have a strong record in inhaled prescription medicine development. There are 13 products currently on the market, launched by our partners and licensees, that Vectura has either developed, or that use technologies that we’ve developed. Our products include a range of DPIs, such as our 60-dose Gyrohaler®, and the flutiform® pMDI, which is marketed by licensees. In addition, leading pharma companies use our formulation technology in their proprietary DPIs, and we have also developed the Breelib smart nebuliser, marketed by a licensee, which uses our device technology.
Looking further back, Vectura has its origins in the late nineties. It was originally a spin-out from the University of Bath (UK), starting out as a CDMO providing formulation development services, Interview primarily focused on the development of inhaled products. Over the years we’ve generally pursued a hybrid model, comprising CDMO services, co-development partnerships and our own proprietary product development programmes.
“When you’re working for a CDMO like Vectura, you work with very diverse organisations, large and small, with all kinds of different entities, all of which are interested in developing medicines, often in disease areas that other companies have less focus on.”
There aren’t many companies out there that can say that they’ve had as much of a hand in all these different technology platforms as Vectura has, including bringing products to market using all of these different platforms.
In terms of my career, I’ve been at Vectura for nearly 16 years, coming from a chemistry background. After leaving academia, I began work at Glaxo, starting off as an analytical scientist, which is how I see myself to this day. I may do a very different job these days, but I think there’s still a lot of that datadriven analyst within me.
I worked on a wide range of inhaled products during the first two decades of my career. I spent a long time working in pMDIs, which were transitioning from CFC to HFA propellants. After that, I started to work on more diverse technologies, such as DPIs and smart nebuliser devices. After Glaxo merged with SmithKline Beecham, I took another role in the inhalation space, where I was responsible for leading the evaluation of new technologies. Ultimately, I became Global Director of Inhaled Science & Technology.
I joined Vectura as a departmental head, working on a range of product development programmes. I now head the Technology Science and Innovation team, which, similar to the work I did at my previous company, involves evaluating new technologies in the inhalation space, as well as progressing product development programmes.
Q Can you expand on your experience of working at Vectura?
A I feel lucky to have had the experience of working in organisations of different scales. In my early career, we were interested in which technologies might enable the next generation of products and, back then, some of the technologies that Vectura was developing interested me. That’s one of the things that made me think of Vectura as an organisation that I might want to work for – it is a high-calibre company that specialises in the inhalation space.
One of the great things about working at Vectura is the breadth of activities that I – and other employees – can be involved in, compared with working at much larger companies. And, of course, when you’re working for a CDMO like Vectura, you work with very diverse organisations, large and small, with all kinds of different entities, all of which are interested in developing medicines, often in disease areas that other companies have less focus on.
Q Let’s discuss Vectura as a CDMO. What is Vectura’s offering to partners?
A Along with that strong track record in device development, we also have an equally strong track record in formulation development – we have more than 200 scientists engaged solely in the development of inhaled products. That is a large group, comparable to the number of people you might see working on the pharmaceutical development of inhaled products for a large organisation. So, while we are a company of about 450 people overall, in my view, we have the same size and power in pharmaceutical development chemistry, manufacturing and control as you might expect to see in a much larger organisation. We have real strength in formulation development, including both for liquids and dry powders, using lactose blending or spray drying to produce engineered particles, which is important for the formulation of biologics.
This is one of the things that makes Vectura special. We’ve designed, developed and brought to market a number of our own device technologies, both in the dry powder space and in the smart nebuliser space. Because of this, we have a proven track record in taking devices literally all the way from cardboard prototypes through to, with the support of partners, fully realised devices in commercial production, prescribed to millions of patients globally. Examples of our marketed devices include the Gyrohaler® and the FOX® handheld, breath-activated, smart vibrating-mesh nebuliser (Figures 1&2).

Figure 1: Vectura’s DPI range includes the Gyrohaler®, F1P, LOMI (Lever-Operated Multidose Inhaler) and OIC (Open-Inhale-Close).
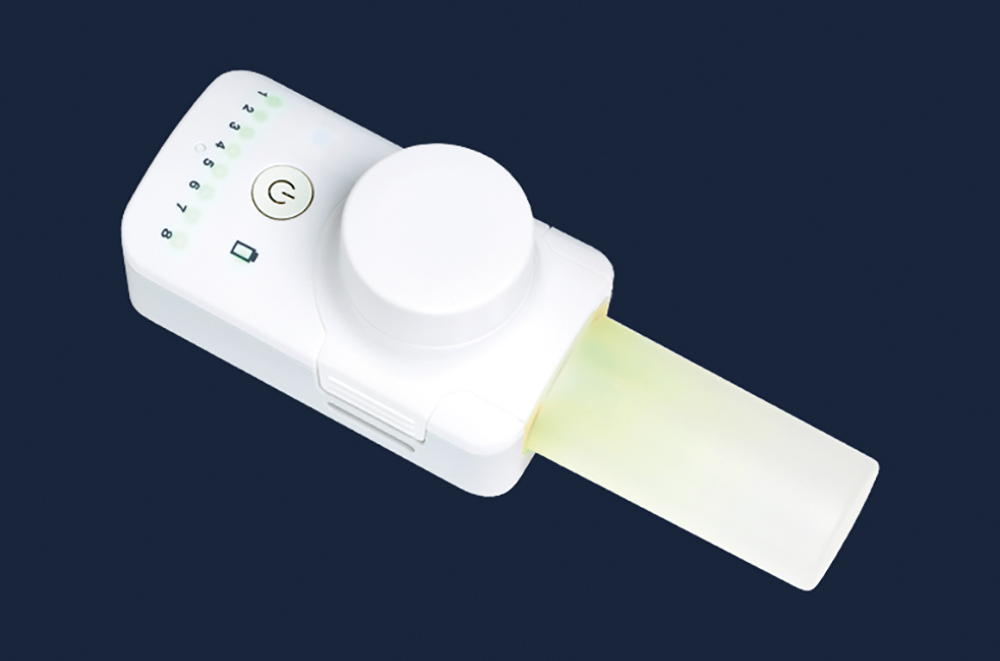
Figure 2: The FOX® handheld, breath-activated, battery-powered vibrating mesh nebuliser. It is CE-marked and is suitable for the delivery of small molecules and biologics, formulated as solutions or nano-suspensions.
“Having the required disciplines under the same roof can really help to solve problems by having experts from device development, formulation, analysis, manufacturing and scale-up all in the same room. Vectura can offer all this.”
While innovating with device and formulation is important, it helps have to have the ability to translate that expertise into working at scale, which is where Vectura’s experience of working with partners to bring products to market really comes into play. If you look at DPIs, which is our most mature platform, we have the ability to work at small scale with tiny amounts of powder; progressively scale up to produce clinical trial supplies for early-phase trials; move on to equipment that’s fully representative of commercial manufacturing for producing late-phase clinical supplies; and finally conduct technical transfer to a commercial manufacturing organisation that will then make the final product.
In addition, we have real strength in regulatory affairs for product development, specifically in increasingly complex devices. Our regulatory team has decades of combined years of experience in this area, highly specialised in inhaled product development.
Q Delving a little deeper into the analytical side of things, could you talk about why the gap between standard lab testing and the reality of how patients use a device matters, as well as how Vectura’s approach to testing addresses that gap?
A Inhaled product testing is onerous (Figure 3). It’s mostly manual. It’s difficult to automate. It generates huge numbers of samples and, therefore, huge quantities of data. There are certain ways in which we’re expected to evaluate inhaled products, in terms of standard regulatory testing. And what most of the testing is about is: “Did the dose come out of the inhaler?” or “What was the particle size distribution of the aerosol delivered from the device?” The size of the aerosol is crucial, of course, as it has a direct bearing on how deeply the medicine may penetrate into the lungs.

Figure 3: Vectura conducts extensive inhaler testing and analysis.
Most of that standard testing is done using a pump, which sucks the powder or the liquid out of the device at a fixed flow rate and delivers it into the equipment that you’re going to use to capture the dose. So, all that data is generated by flicking a switch and turning a pump on and off. Often, however, it’s not at all representative of what a patient really does when they use a device, let alone a patient who might have impaired lung function or a restrictive lung disease.
Also, I think the other thing about all of that routine testing is that the volumes of air that you are using to suck the dose out of the device are not always representative of patient lung volumes. For example, if you’re doing standard cascade impaction testing, you typically suck four litres of air through the equipment. It’s difficult to imagine a person of any size with a four-litre inhalation volume, so it’s not that representative of the patient-use case.
As soon as you’re thinking about evaluating an inhaler in an early clinical study, you want to know what might happen when a patient uses the device. To really understand what’s going on, you need to use more realistic testing using all the previously mentioned tools together with in silico tools, such as lung deposition modelling, where you introduce the aerosol into a mathematical model to represent the set of patient lungs, or even a “real” lung model derived directly from patient CT scan to get a much better feel for lung deposition.
It’s now possible to get a comprehensive picture of what happens when a patient uses the device and develop an understanding of how that potentially translates to blood levels. Building this understanding can save an enormous amount of time and money during development.
Q Outsourcing development is a highly competitive space, including in the inhalation space – what makes Vectura stand out amongst the competition?
A At Vectura, we have all the disciplines needed to progress an inhalation project from the very early stages of development to ready for commercialisation. We are effectively a one-stop shop for our customers.
Having the required disciplines under the same roof can really help to solve problems by having experts from device development, formulation, analysis, manufacturing and scale-up all in the same room (Figure 4). Vectura can offer all this, with our expertise spanning DPIs, nebulisers and pMDIs. We’re also currently moving into the intranasal sector as well.

Figure 4: Having all the disciplines required for a development programme under the same roof can really help to solve the particularly tricky challenges that are always present in inhaled product development.
When someone approaches us with an idea for a product, we can look at their target product profile and give them our best, unbiased advice, even if that means using a third-party device instead of one of ours. I think that’s another strength we have – we’re not constrained to going down a particular approach, we will propose what we think is best for the programme regardless.
“There’s substantial interest in the intranasal route for vaccines, but there’s also excitement around using intranasal for acute care applications.”
Q For a long time, asthma and COPD were seen as the mainstay of the respiratory sector. However, in recent years, the industry has showed increasing interest in using the inhalation route to tackle a much wider range of disease areas – can you offer us any insights on this trend?
A There is, of course, the massive trend towards biologics. We use pipeline analysis databases to view all of the inhaled products currently in development, so we can work out what that says about the future. Broadly speaking, there are usually 700 or more inhaled products in development across the world at any one time. We track how those change and evolve over the years and, last year, for the first time ever, we saw a switch from small molecules to the majority being biologic products. Also important to note is that around a third of those products are intranasal, which says something about the massive opportunity intranasal delivery represents.
There are good medicines in mainstream asthma and COPD now. There are definitely still some intractable areas of those diseases, so there is still scope for innovation, but in mainstream healthcare, the issues relate more to people taking their medicine regularly or to having access to good education to enable them to use their inhaler device correctly. Hence we see interesting things happening with regard to connectivity and education to improve adherence and inhaler-use outcomes.
Currently, there seems to be interest in systemic delivery via the lung alongside niche and orphan respiratory diseases getting a lot of attention from smaller biotech companies. The covid-19 pandemic generated interest in treatments that could potentially alleviate symptoms for people suffering from severe diseases, and covid-19 got people thinking about all sorts of different potential therapeutics.
There’s also interest in vaccine delivery via the nose or lungs. There could be some major advantages to the delivery of vaccines to the respiratory system, such as removing the need for cold chain storage. If you can have a room-temperature-stable dry powder that you can ship all over the world and inhale via a simple, low-cost device, that’s going to be hugely beneficial in difficult-to-reach regions.
Q Let’s move on to another current trend in inhalation, this time on the device side. As you’ve mentioned, Vectura has developed a proprietary smart mesh nebuliser, FOX. Why is there such heightened interest in mesh nebulisers and soft mist inhalers?
A A lot of the interest is driven by two things. One thing is the desire to get excellent deposition in the lung and, in particular, the small airways. Say you’re trying to treat idiopathic pulmonary fibrosis, the disease is deep down in the lungs, so you have to get the therapy as deep into the lungs as you can. The second thing is that biologics tend to be aqueous soluble, which means that, if you want to get to the clinic for a fast proof of concept, ideally you’re going to want a device that can deliver an aqueous solution. That way, there’s no need to pursue a complex formulation that might require huge amounts of material – you’ve got your liquid solution, you stick it in the device and you give it to people. It’s fast, it’s simple, it’s cost effective and it maximises the probability of success via excellent lung deposition.
Those are, in my opinion, the two main reasons why there’s a massive interest in Vectura’s FOX technology and mesh nebulisers more generally, as distinct from jet nebulisers, which are noisy and bulky. Also, the mesh nebulisation process is more gentle, which is important when you’re dealing with fragile complex biologic molecules.
On top of that, FOX has a number of unique features compared with other mesh nebulisers. For example, a standard mesh nebuliser constantly produces aerosol, regardless of whether the patient is breathing in or breathing out, which means half of the medicine is wasted with those devices. FOX, on the other hand, only generates aerosol when the patient is inhaling, so there’s none of that waste.
The other thing that FOX does is guide the patient to inhale at a fixed flow rate, typically 15 L/min, to maximise lung deposition. Compare that with normal, continuously producing nebulisers, where patients sit with the device mouthpiece constantly in their mouth and do tidal breathing, which is a relatively shallow inhalation manoeuvre.
What FOX is trying to get the patient to do is draw the aerosol as deep down into their lungs as they can to get the best results from their medication. To achieve this, FOX has to have some resistance to air flow, which is variable – the harder the patient tries to suck on the device, the more the device restricts flow. This results in the patient ending up in a comfortable space for their optimised inhalation flow, and there are lights in the mouthpiece of the device to help guide the patient to be as close to 15 L/min as possible. We’ve also implemented Bluetooth connectivity in FOX, which enables it to be connected to an app to transfer data, which can be used in a clinical trial or commercial setting.
It isn’t a one-size-fits-all solution for every medicine in development – that doesn’t exist – but, at certain stages of development or for certain kinds of medicines where maximising lung deposition is important, we think FOX is an excellent solution.
Q To wrap up, please could you share your thoughts on the major changes and innovations you expect the respiratory sector to see over the coming years?
A I think connectivity is a big thing. If you look at conferences over the past five years, there’s been a significant focus on connectivity – it’s something people are very interested in. However, I think there are still some questions around who’s going to pay for it. I also think the strongest case for it is in the clinic to start with, where connectivity can help you understand what individual patients have done during the study, which can help you decide how usable their data is – if they haven’t used the device properly, it could mean that their data is poor, and connectivity can tell you why.
High-dose therapies is an area that I think could be key in the respiratory space. We’re already moving towards higher doses, partly driven by biologic therapies, so you are delivering tens or hundreds of milligrams instead of 50 or 500 μg, which is the dose for a potent asthma molecule. This means that there’s a step change in how much you have to deliver.
Another driver is the sheer diversity of different kinds of illnesses and medicines that companies are evaluating these days. We’ll see a lot more biologic therapies coming through the pipeline. And, as I’ve said, there’s substantial interest in the intranasal route for vaccines, but there’s also excitement around using intranasal for acute care applications. Opioid overdose is a key example, where the patient may be unconscious and the easiest way to deliver emergency recovery medicine is for a caregiver to spray it up the patient’s nose.
Lastly, I’d note that there’s growing interest in using the inhalation route for psychiatric medicines – treatments for autism, for example, and the use of psychedelics in conjunction with intensive therapy to help people overcome things like addiction and post-traumatic stress disorder. There are lots of ideas out there for new and different kinds of medicines. It’s a truly exciting area to be working in.
To discover more about Vectura’s expertise in inhaled drug development and manufacture, visit: www.vectura.com.

