Citation: Piera P, Bauer R “Manufacturing DPIs: Case Study of IMA Adapta® With Boehringer Ingelheim Spiriva®“. ONdrugDelivery Magazine, Issue 102 (Nov 2019), pp 32-36.
Pietro Piera and Rainer Bauer investigate the optimal process parameters for low-dose dry powder inhalers achieved by dosator technology, presenting a case study in which IMA’s capsule filler, Adapta®, is used to fill Boehringer Ingelheim’s Spiriva® (tiotropium) dry powder inhaler.
“The key to achieving optimal filling and control of low-dose dry powder for inhalers is combining the dosator technology and the direct gravimetric net weight control.”
In 1948, the first commercial dry powder inhaler (DPI) device was launched on the market. This first technology seems archaic by today’s standards: a deep inward breath would cause a ball to strike a cartridge containing powder and shake the powder into the airstream. Since then, changes in the drug delivery market and regulatory pressures have driven innovation of DPIs forward.
It is estimated by the WHO that, worldwide, some 300 million people suffer from asthma and 240 million people suffer from chronic obstructive pulmonary disease (COPD). DPIs represent 50% of the total asthma/COPD market by value worldwide. The latest patient-focused studies using DPIs indicate that the expectations regarding this technology have evolved. Patients and pneumologists are now increasingly focusing on convenience and ease of use, favouring a compact design. Indeed, DPIs have shown great promise in their ability to deliver drugs reliably and effectively, and novel designs can ensure that future cost, compliance and safety challenges are overcome.
Some of the performance characteristics essential to DPIs are related to dose delivery, fine particle fraction content and performance levels at varying airflows. These characteristics can differ from one powder formulation to another, and some fine tuning of either device or formulation – or a combination of both – may be necessary to achieve optimal performance. Micro-dosing DPIs takes this challenge to extremes.
“Patients and pneumologists are now increasingly focusing on convenience and ease of use, favouring a compact design.”
When producing pharmaceutical products for DPIs, industrial manufacturing aspects must be considered together with optimisation of the process to achieve a reliable control method. Achieving precise micro-dosing, gravimetric weight control, containment measures and ease of device assembly are typical challenges which could be faced.
Direct weight control is performed in-line on each single capsule, both before and after filling. IMA draws on its expertise to provide advanced solutions for DPI processing and capsule filling. For example:
- Absence of mechanical powder compression for improved airway intake.
- Accurate micro-dosing and automatic feedback and adjustment.
In this article, we investigate optimal process parameters for low-dose DPIs achieved by dosator technology. We show that a major advantage of using dosators for processing DPIs is that they can be accurately adjusted without any need to compress or aspirate the powder.

Figure 1: Adapta® 100, IMA’s dosator capsule filling machine with 100% gravimetric net weight control.
CASE STUDY: SPIRIVA® PRODUCTION
The aim of the study was to explore the best process parameters to achieve a 5.5 mg dose of a powder mix including a lactose carrier, and long-acting brochodilator tiotropium bromide, which Boehringer Ingelheim markets as Spiriva®.
Boehringer Ingelheim initially carried out the process on various different capsule filler types and then optimised it thanks to IMA capsule filling machine model Adapta® 100 (Figure 1) with 100% gravimetric net weight control.
Materials
Components of the case study are:
- Blend of lactose-based carrier and tiotropium bromide (Spiriva®)
- Adapta® 100 – an industrial-scale production capsule filler implementing dosator needle technology together with gravimetric 100% net fill weight checking system with scales resolution < 0.01mg.
Methods
The first steps of the study were conducted by Boehringer Ingelheim alone. Several capsule filling machines were tested, with a range of processing technologies (continuous, intermittent motion), dosing systems (dosator needle, vacuumed drum filler), and systems for mass control (capacitive sensors, elastomers for gravimetric weighing).
The processing technology did not have a direct impact on performance, unless needed for other features such as gravimetric weighing. The dosator needle was preferred when compared with drum filler for the following reasons:
- Dosator fills the dosing chamber effectively. The drum filler relies on the force of gravity to fill the chamber (ineffective and difficult to control) and vacuum (irregular since air follows preferential routes inside the powder, creating a “rat hole”, and the membrane soon clogs).
- Dosator holds micronised powders in the chamber thanks to their cohesiveness and very small dosator diameter. In addition, IMA applies a patented syringe effect. Vacuumed drum filler relies on the vacuum to hold the powder in the chamber, thin particles are aspirated and this generates high losses of product and frequent stops.
- Average weight centred on the target weight. The chamber height of each dosator can be accurately set and individually adjusted.
Figure 2 shows the weighing statistics for the total batch (T) and for each dosator individually.
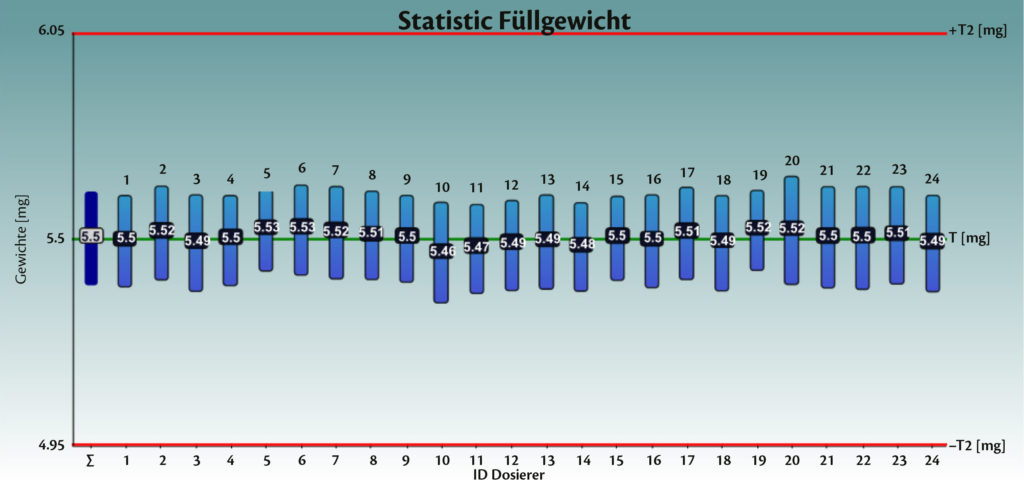
Figure 2: Weighing statistics for the total batch (T) and for each dosator individually.
Analysis of the process
The second step of the study was conducted by IMA and Boehringer Ingelheim. After the pre-runs, the process was analysed and studied in deep detail. IMA and Boehringer Ingelheim put in place people specialised in mechanical design, statistics, and mathematics analysis and software development. Several tests were performed at the IMA factory on Adapta® with 100% gravimetric net weight control. The process analysis loop was followed as described in Figure 3.
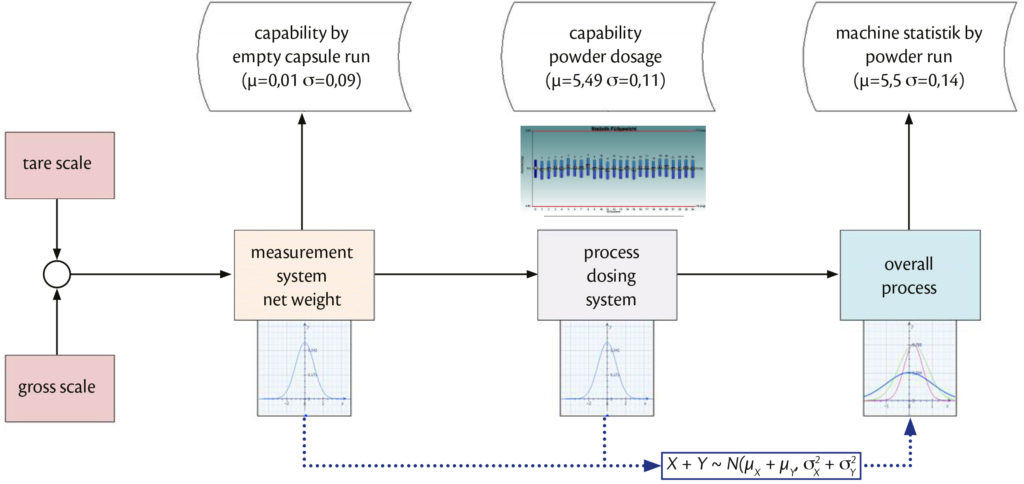
Figure 3: Process analysis loop.
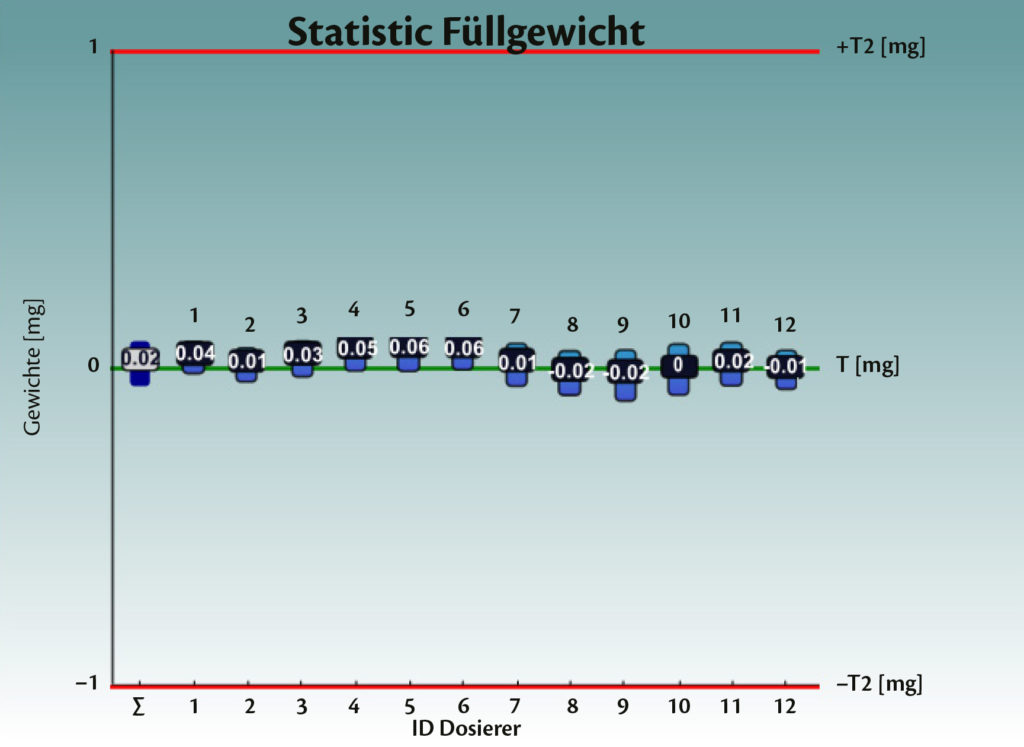
Figure 4: Test with empty capsules on Adapta® 100 with 100% gravimetric net weight control.
The pre-runs showed that Adapta® was fully capable of handling Spiriva® capsules and that the dosing by dosators was perfectly achieving the requirements for the product. Boheringer Ingelheim worked together with IMA to find the right dynamic parameters and optimise the closed-loop control.
The weighing system was optimised. Several tests were performed when no powder was dosed (Figure 4). The “ideal” system should result in a net weight equal to zero, since the capsule is empty. The standard deviation represents possible errors in scale accuracy and air flows, for example, due to the vacuum opening, vibration, etc.
The timing for the weight sampling was changed and the calibration weight was set to 100 mg (tolerance class E2). Figure 5 shows the results achieved. This provides feedback and an evaluation method for the weighing method itself.
The joint work demonstrated that a perfect dosing system needs to be controlled by a perfect weighing system (Figures 4 and 5).
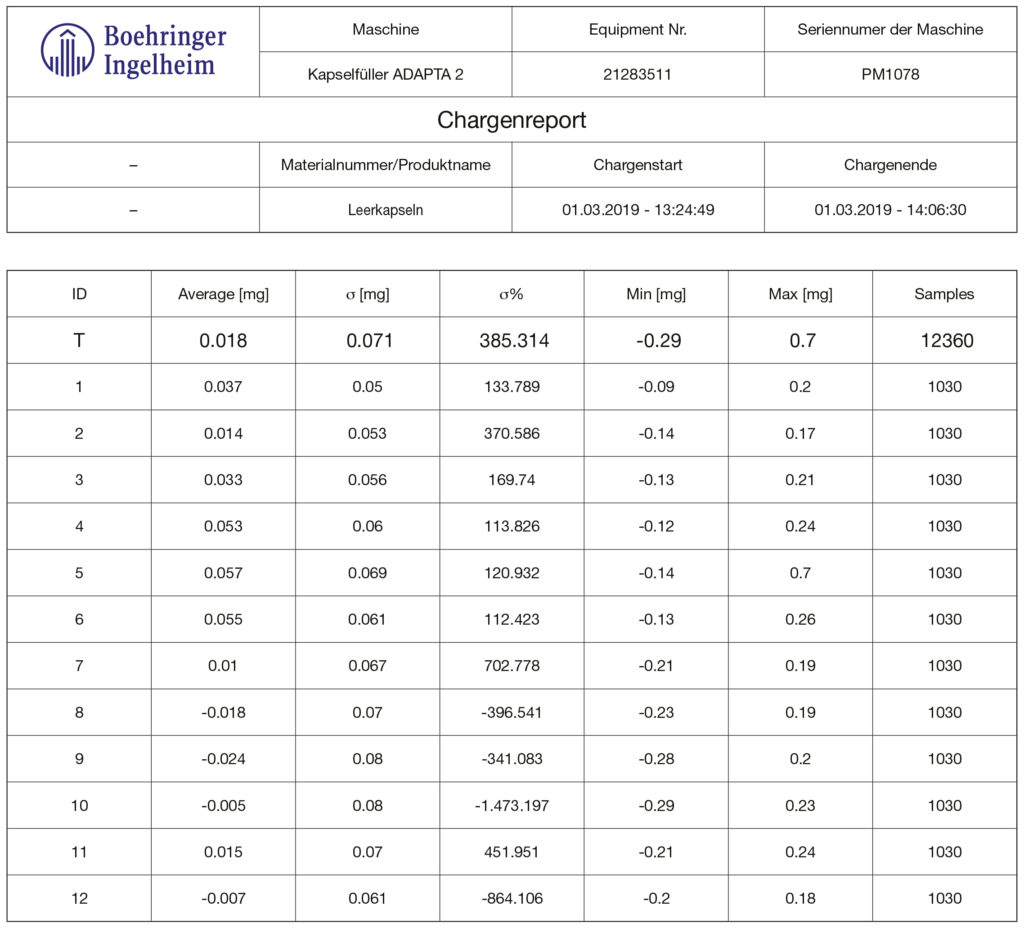
Figure 5: Test with empty capsules on Adapta® 100 with 100% gravimetric net weight control.
Process requirements
- Capsule size 3
- Powder for inhalation
- Net fill weight 5.5 mg +-10% ➔ LSL = 4.95 mg, USL= 6.05 mg
- 100% control for filling
- Smooth capsule run
- Easy to use – fast setting up, cleaning and operation
- Production data accessible.
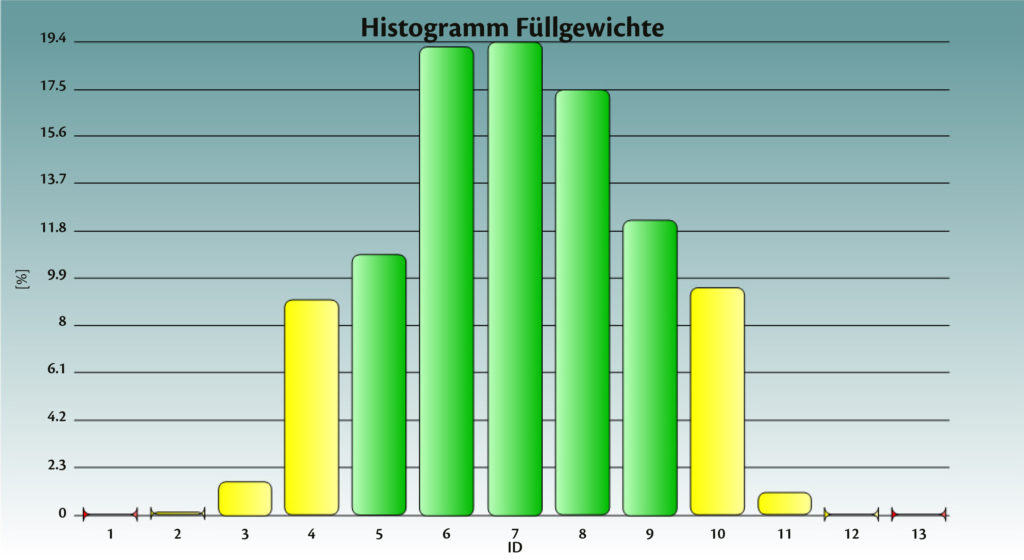
Figure 6: Spiriva® achieved fill weight on Adapta® with 100% gravimetric net weight control.
Technical criteria
- Machine speed
- Machine size
- Machine kind (intermitted pulsed / continuous run)
- Filling technology (dosator needle, sliding chamber, vacuumed drum)
- Capsule handling: opening / move (body, cap) / close
- Machine complexity (easy to run)
- Set up and disassemble speed
- GMP design (surfaces / materials / easy to clean / no dead room)
- Measurement system (principle / stability / influences)
- Sold machines in the market (support, developed to use)
- Costs (invest, maintenance, media).
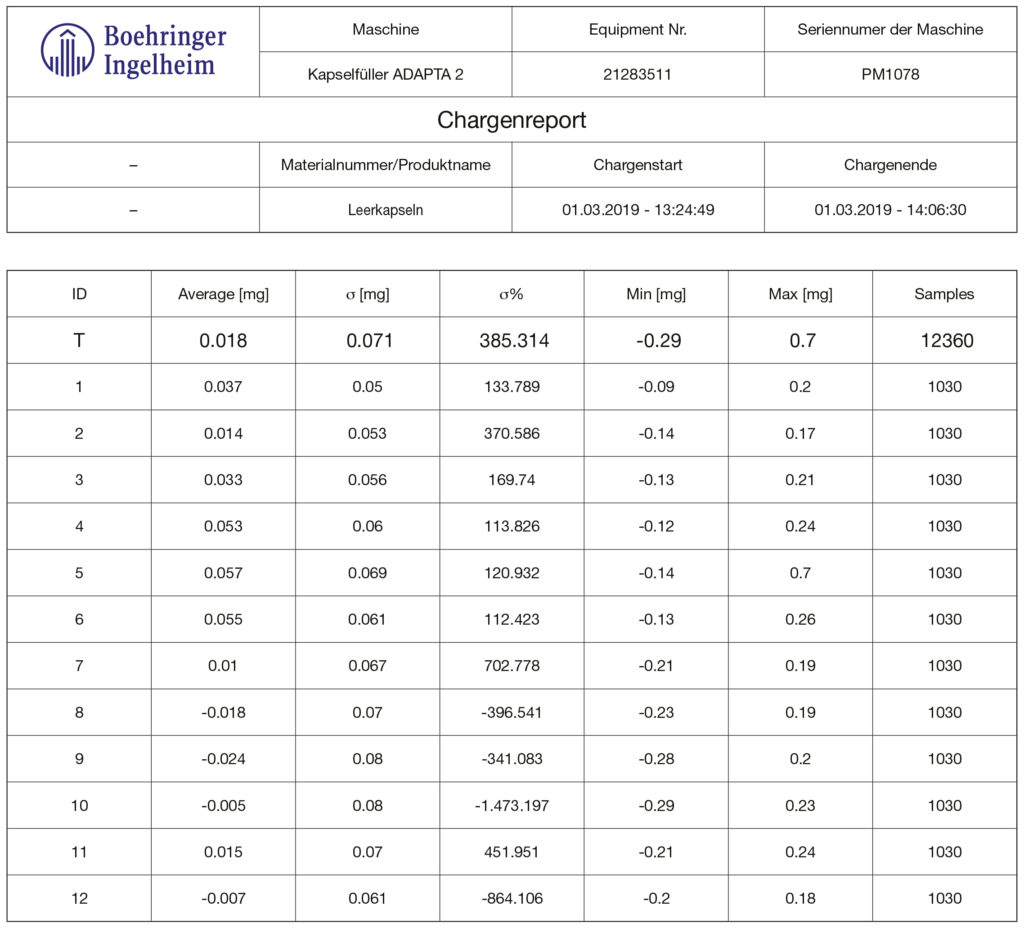
Figure 7: Spiriva® achieved fill weight on Adapta® with 100% gravimetric net weight control.
Results
Figures 4-7 show the achieved fill weight for the total batch (“T”) and for each dosator individually – perfectly centered and on target (μ= 5.5 mg and bias= 0.00 mg). After several sessions of trials, machine parts optimisation, deep analysis of the measuring system and its synchronisation with the capsule filling process, Adapta® with 100% gravimetric net weight control was able to perfectly match process capability requirements with very low target dosage. And in particular Adapta® is able to incorporate:
- a very accurate and reliable system for auto-diagnosis when handling with empty capsules, able to achieve:
– Standard deviation σ <0.1 mg
– Bias -0.03 to +0.03 - a very stable and reproducible system for dosing DPI, able to achieve:
– Standard deviation σ= 0.13 to -0.16 mg
– Totally centred on average, with bias 5.5 mg +/-0.05 mg
Conclusion
As shown by this study, a major advantage of using dosator technology for processing low-dose DPIs is that the system can dose very small amounts of powders into capsules. This powder-dosing technology does not require powder compaction to transfer the powder to the capsule, ensuring that the powder within the capsule is less likely to form aggregates and is maintained as a free-flowing powder. Maintaining the free-flowing properties of the dispensed powder within the capsule better ensures the release of powder from the capsule into the inhaler when the capsule is pierced – thereby better controlling both the emitted dose and the fine particle fraction of the dose discharged from the DPI.
The key to achieving optimal filling and control of low-dose dry powder for inhalers is combining the dosator technology and the direct gravimetric net weight control. This is available on an industrial production scale capsule filler, Adapta®.
REFERENCES
- Edwards D, “Applications of capsule dosing techniques for use in dry powder inhalers”. Ther Deliv, 2010 July, 1(1), pp 195–201.
- Rogueda P, “Take a deep breath. Inhalable drug delivery”. World Pharmaceuticals, April 2016.
- Williams G, “The future of DPIs: Aligning Design with Market Demands”. Drug Development & Delivery, December 2012.

