Citation: Williams N, “Next-Generation Connected Drug Delivery Supports Data Liquidity & Cost Savings”. ONdrugDelivery Magazine, Issue 103 (Dec 2019), pp 32-35.
Neil Williams discusses medication non-adherence, the toll it takes on the healthcare system and how integration, analytics and more affordable connectivity in drug delivery devices as part of a connected health ecosystem improves patient care and lowers costs.
The issue of medication non-adherence has long been raised as a global challenge that not only has a deleterious impact on patient outcomes but also creates a large burden of cost to the healthcare system. With accountable care organisations (ACOs) and payment-by-results agreements springing up rapidly, value-based care is no longer a vision but a reality. The pay-for-performance model has created an incentive-based environment where payers no longer just reimburse providers to manage a patient’s condition during a finite snapshot in time. When providers can show progress over the long term and demonstrate a reduced burden of unnecessary costs and deliver demonstrable benefits to all stakeholders, they’re eligible to receive a stipend for the savings created. In this sense, the outcome now becomes the income.
“The pay-for-performance model has created an incentive-based environment where payers no longer just reimburse providers to manage a patient’s condition during a finite snapshot in time.”
More than ever, providers need to be able to monitor medication usage and, more importantly, measure changes in a patient’s health status. Statistics show that up to 50% of medications are not taken as prescribed and that 33% of US hospital admissions are due to poor medication adherence.1
Drug adherence, while important, is only part of this equation. What’s needed today is a much broader, more holistic view of the patient. Metadata and big data can show not only whether a patient was taking a medication on time as prescribed but also multiple factors that contribute to that individual’s overall health and well-being.
DIGITAL HEALTH IS THE NEW NORM
This is where connected health comes in. Sensor-embedded devices that are part of a connected health ecosystem and can digitally transmit data back to the patient’s electronic health record through an app on their smartphone – and automatically alert providers of any issues or inconsistencies – have come a long way. Currently, there are more than 165,000 health-related apps available on iOS and Android, and that number is increasing. The growing popularity of wearables, home-use scales, blood pressure monitors, glucose meters and drug delivery devices that measure vital signs and adherence rates can offer a remote glimpse into a patient’s health status.
The potential for capturing a more all-inclusive perspective of the patient through digitally connected drug and monitoring devices looks promising but it’s still maturing as the “Internet of Medical Things” (IoMT) evolves. As more patient data is collected, moved into the health system and shared back out to patients from providers, it becomes that much more valuable. Essentially, this “data liquidity” allows patients to commission their data to their providers and receive professional guidance to tailor individual treatment more finely.
“The potential for capturing a more all-inclusive perspective of the patient through digitally connected drug and monitoring devices looks promising but it’s still maturing.”
While the world has come to expect digital health as the norm, strides are under way by global leaders like Apple, Google and many others to make data liquidity that much more accessible. Just recently, Google announced its acquisition of Fitbit, a pioneer in wearables, to continue advancing this category by delivering innovative, affordable and engaging devices. Being “on Fitbit” is not just about the device – it represents an immersive experience from the wrist to the app, designed to help people understand and change their behaviour.
In a similar fashion, embedding connectivity in drug delivery solutions like inhalers, injectors, patch pumps and infusion devices enables patients and healthcare professionals to track device status, as well as when patients are taking their medication and the dosage amount. Advantages of shared data through device connectivity include increased patient feedback, improved targeting of clinician support and the delivery of actionable insights. Furthermore, connectivity provides valuable opportunities to engage and support patients through reminders, incentives and peer communities to improve adherence. For example, Phillips-Medisize’s cloud-based connected health platform (Figure 1), which builds on the success of the first US FDA-approved connected autoinjector device, facilitates this secure data sharing between provider and patient.
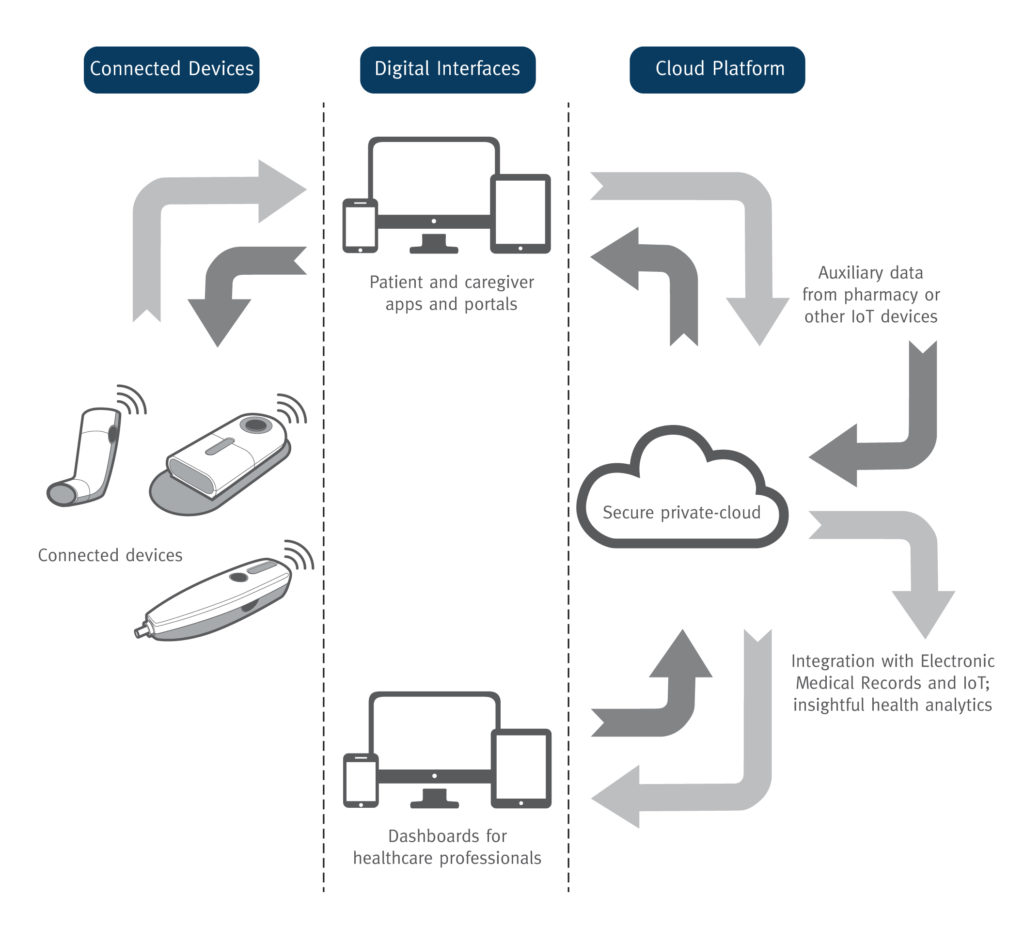
Figure 1: The Connected Health Platform by Phillips-Medisize encompasses extensive information-sharing, analytics capabilities, robust cybersecurity and streamlined regulatory documentation to support pharmaceutical, medical device and diagnostics companies worldwide.
INTEGRATION & ANALYTICS: KEY TO HOLISTIC PATIENT VIEW
As progress is being made toward greater data liquidity through connected wearables, monitors, drug delivery devices and more, there are many more touch-points involved in capturing and transmitting patient information. Ideally, the goal is to ensure this flow of data is integrated directly into a patient’s electronic health record – not just in isolation but consolidated with all the other multiple data points in the full digital ecosystem to create a 360° view of the patient. A connected health platform should combine a reliable analytics tool with a powerful integration engine that integrates patient data with electronic medical records and other data from pharmacy, mHealth and IoMT devices.
Analysing this cumulative data can ultimately provide valuable insights that may help drive better patient outcomes on an individual level as well as across patient populations, such as those with chronic diseases. By leveraging analytics, providers can begin to identify outliers, intervene earlier, steer patients toward behavioural changes and deliver more personalised care tailored to the individual. Everyone benefits – the patient, the provider and the payor – as a result of improved medication and disease management, which reduces the burden of cost, which can improve outcomes, reduce co-morbidities and the overall cost of care.
The global cost of not enabling data sharing through digital health is significant. On the flip-side, connected healthcare has the potential to create up to US$450 billion (£350 billion) in savings in the US alone. In a McKinsey consumer health insights survey, 68% of 14,500 respondents reported behavioural change as a result of using devices and services to manage chronic conditions.2 Greater patient engagement and increased data liquidity, empowered by connected health solutions, therefore helps solve a widespread human problem and drives inefficiency out of the healthcare system.
Even though connectivity is a relatively recent innovation in drug delivery devices, the benefits are clear and important to the entire healthcare industry. Greater adherence has the potential to increase drug sales and provide a return on investment to pharma companies who typically bear the additional device and service costs.

Figure 2: The smart, reusable autoinjector can handle multiple drugs through a syringe RFID reader and has an intuitive user interface
with illuminated user graphics and audible feedback.
As today’s drug delivery devices continue to evolve from purely mechanical in design and function to more sophisticated solutions that embed electronics (Figure 2), there is a trend toward adding connectivity to support data sharing. Adding connectivity to next-generation devices, however, has been met with some resistance by medical device companies, who are under increasing pressure to keep manufacturing cost down.
COST-EFFECTIVE CONNECTIVITY IS A REALITY
The initial manufacturing cost of integrating connectivity into a drug delivery device can be high. Adding even $3 to the manufacturing cost of an insulin injection pen translates into roughly a seven-fold increase in cost per unit and, for a low margin medication, it is prohibitive. This additional cost can’t realistically be recouped through price increases.
One way to make connected medical devices more economically viable is to rethink the initial approach to product design in order to reduce manufacturing expenditures for a lower cost per unit. Simply put, how can companies lower the cost of integrating connectivity into drug delivery devices as a viable alternative to a bulky add-on connectivity device to achieve an affordable price point, especially for those with higher production volumes?
Phillips-Medisize is an example of an outsourced manufacturing partner that benefits from Molex’s electronics capability and ownership. The combined businesses benefit from a dedicated low-cost connectivity project team including mechanical, electronics and embedded software engineers, as well as app designers and human-factor specialists, all focused on market- and customer-specific needs. By leveraging their collective industry expertise and specific skill set in device development, the team is focused on one goal – to successfully integrate connectivity features into drug delivery devices at a lower cost than previously considered possible. Given the new level of affordability, incorporating connectivity even in disposable devices is now possible.
CONCLUSION
Pharma companies are under growing scrutiny from regulators and health insurers to do more to demonstrate the value of their medications, which puts increased pressure on drug delivery device manufacturers to rise to the challenge – all while saving costs.
In the end, connected health solutions should be useable and affordable to meet industry, provider and patient needs – no matter if it is for a common disease or a complex rare disease. Successful products are built on three essential foundations: robust technology, solid business planning and empathetic patient engagement. Connectivity technology promotes data liquidity by providing an effective and efficient way to collect patient information and capture insights that inform better, two-way decision making.
If we are to raise patients’ medication adherence, it is essential that we succeed in creating a 360° focus on patients, caregivers and healthcare providers and their interactions, as well as catering to the full ecosystem. To accomplish this, we need a well-functioning, reliable connected health system that embraces all aspects of digital health.
REFERENCES
- Osterberg L, Blaschke T, “Adherence to medication”. N Engl J Med, 2005, Vol 353(5), pp 487–497.
- “Unlocking Digital health”. Research Report, McKinsey, April 2015.



