Citation: Ward D, “Optimising Nasal Drug Products for Systemic Delivery”. ONdrugDelivery Magazine, Issue 106 (Apr 2020), pp 56-59.
David Ward discusses the benefits of systemic nasal delivery, describes a number of formulation strategies, and explains how to optimise absorption through properly informed formulation and device selection.
Nasal sprays are non-invasive and generally well tolerated by most patients, which drives a relatively high patient compliance rate compared with other more invasive and painful delivery routes.
Historically, nasal sprays have been used primarily for the treatment of topical conditions such as seasonal rhinitis (hay fever), cold symptoms and sinusitis, where the systemic absorption of these drugs is undesirable due to effects that could occur to the hypothalamic–pituitary–adrenal axis, bones, eyes or other parts of the anatomy.
|
INN (Proprietary names) |
Therapeutic Target | Stage |
| Sumatriptan (Imigran,Tosymra) | Migraine | Marketed |
| Calcitonin (Miacalcin, Fortical) | Osteoporosis | Marketed |
| Naloxone (Narcan, Evzio, Nyxoid) | Opioid overdose | Marketed |
| Oestradiol (Aerodiol) | Hormone replacement | Marketed |
| Midazolam (Nayzilam) | Epileptic seizures | Marketed |
| Diazepam (Valtoco) | Epileptic seizures | Marketed |
| Esketamine (Spravato) | Resistant depression | Marketed |
| Live attenuated influenza vaccine (Fluenz Tetra/FluMist) | Influenza | Marketed |
| Levodopa, Glutathione, Nicotine, Insulin |
Parkinson’s disease | Clinical |
| Insulin | Alzheimer’s disease | Clinical |
| Testosterone | Anxiety | Clinical |
| Betahistine (AM-125, AM-201 Auris Medical) |
Medical) Vertigo, antipsychotic-induced symptoms |
Clinical |
| Lorazepam (NRL-2, NRL-3, NRL-4 Neurelis) |
Acute anxiety, status epilepticus, psychomotor agitation | Clinical |
Table 1: Examples of nasal delivery products on the market and in development.
More recently, there has been increased interest in delivering drugs to the nose for systemic conditions, with products already successfully marketed for the treatment of migraine, osteoporosis, the reversal of opioid overdose, hormone replacement, epileptic seizures, depression and flu vaccinations. There is also interest in nasal delivery for the treatment of Parkinson’s, Alzheimer’s, anxiety, antipsychotic-induced weight gain and vertigo (Table 1). A range of therapeutic agents such as proteins, peptides and nucleic acid-based agents are being considered for delivery by non-invasive routes such as nasal, however, a major concern for some of these new therapeutic agents is their poor absorption characteristics.
WHY CHOOSE SYSTEMIC NASAL DELIVERY?
There are several advantages of the nasal route. The different tissue types in the nasal cavity allow for systemic delivery, possible nose-to-brain delivery and access to the lymphatic system for vaccines and biologics. This means that nasal delivery can be used to avoid parenteral administration of some compounds, with relatively rapid absorption that also has the benefit of avoiding the hepatic first-pass effect, where the therapeutic agent is rapidly metabolised by the liver into inactive components, therefore, reducing efficacy. The method of delivery is also a simple process so leads to good patient compliance as actuating a device into the nose is preferable to most people than having to inject themselves.
“Strategic formulation development can be used to increase residency time of the active in the nasal cavity.”
As with other routes of administration, there are some disadvantages to nasal delivery. The nasal anatomy, by design, is quick to clear material from entry to the airways via mucociliary clearance. This is where the cilia covering the nasal mucosa drag mucus and deposited material from the front of the nose to the throat where it is swallowed. This means there is typically a short window for absorption to occur. The natural nasal cycling of the nose can also affect absorption rates – this is an approximate two-and-a-half-hour cycle where one side of the nose is more congested than the other, with the process alternating between sides. So, if your dose consists of only one shot into the nose, then absorption could vary depending on which nostril is used.
Similarly, many people have deviated septa which can change the deposition properties on each side, and we must also consider that everyone’s nasal geometry is slightly different and inconsistent absorptions of the drug product – for example, caused by infections blocking the nasal passages – will occur.
Simplifying the nasal anatomy, there are broadly three main areas of interest. First, the turbinates, which have a large surface area and can therefore be used for systemic delivery. Second is the olfactory region at the top of the nasal cavity, which is responsible for our sense of smell, but could also be useful for direct nose-to-brain delivery of particular treatments, such as those for migraine, Parkinson’s or Alzheimer’s, or any molecule that cannot pass the blood/brain barrier. Thirdly, towards the very back of the nasal cavity there is nasal associated lymphoid tissue, which is connected to the lymphatic network and can induce a mucosal and systemic immune response, so is therefore a good target for delivery of vaccines and biologics.
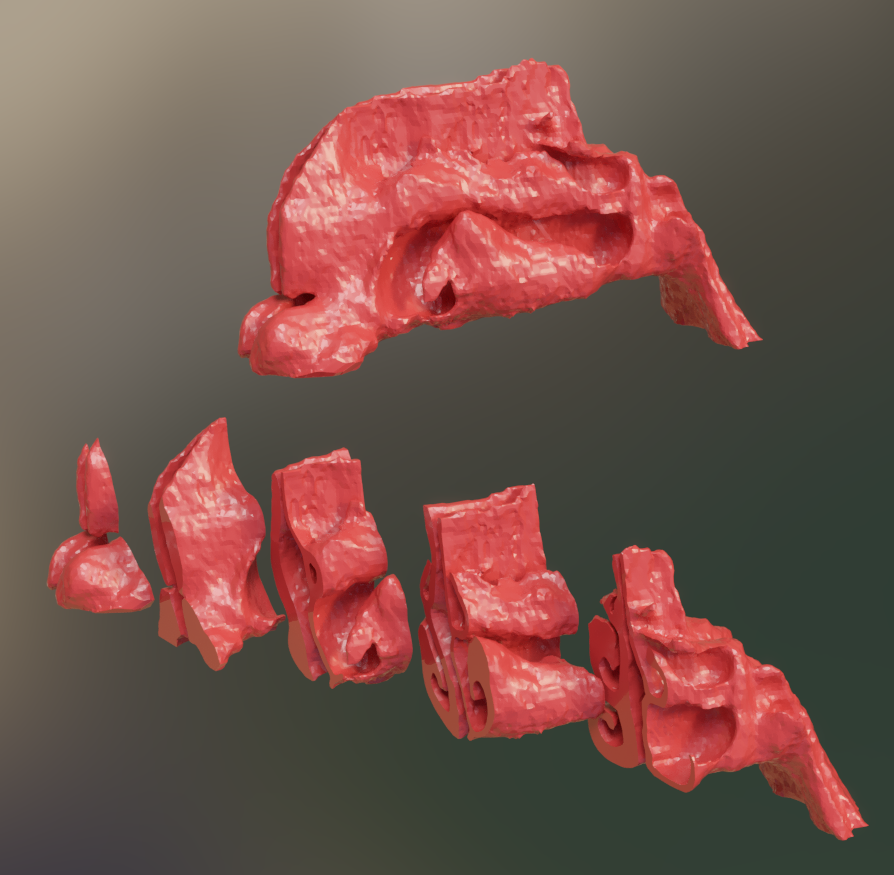
Figure 1: MRI cross section of nasal cavity.
“There are three routes to help optimise systemic absorption, two of which are formulation based and the third involves device selection.”
A sectioned solid representation of the nasal cavity is shown in Figure 1 – generated from MRI scans of the head. It shows, from the left, the nostrils leading to the nasopharynx and throat to the right of the image, which illustrates how complex the structure of the nasal cavity is. It comprises a network of very narrow passageways, including two narrow slits at the front of the nose, called the nasal valve, where much of a nasal spray is deposited, particularly in the case of traditional aqueous nasal sprays, although some other types of device can have higher deposition in the more posterior areas.
Other limitations of nasal delivery include low permeability of the nasal tissues for high molecular weight therapeutics, solubility of the API, pH and lipophilicity of the drug and also the presence of proteolytic enzymes that may give rise to degradation of the drug substance in the nasal cavity. Lipophilicity is specifically relevant for biologics, where engineering to improve lipophilic properties of the biomolecule can lead to loss of structural integrity whilst susceptibility to enzyme activity can lead to degradation.
To help overcome these challenges, there are three routes to help optimise systemic absorption, two of which are formulation based and the third involves device selection.
OPTIMISING SYSTEMIC ABSORPTION THROUGH FORMULATION
Strategic formulation development can be used to increase residency time of the active in the nasal cavity using either bioadhesives or viscosity adjusters to slow down the rapid mucociliary clearance in the nose and increase the amount of drug delivered.
Common excipients include natural polysaccharides which show interesting biological properties, including biocompatibility, biodegradability and bioadhesion. A key example is chitosan which has been used in several trials but is not in any marketed products to date. Another bioadhesion agent is carboxymethyl cellulose. A mixture of carboxymethylcellulose and microcrystalline cellulose is commercially available as Avicel RC591 (DuPont) which forms a non-Newtonian fluid that is free flowing when being mixed or sprayed but then forms a thick gel following actuation. This time-dependent shear thinning behaviour helps uniformity of content when mixed, accurate dosage and ease of sprayability for nasal sprays. There are also common thickening excipients such as polyethylene glycol, polyvinylpyrrolidone and glycerol.
To enhance the absorption of poorly permeable drugs, another strategy is to use permeability enhancers such as Neurelis’s Intravail (n-dodecyl beta-D-maltoside) which is included in marketed products of sumatriptan (Tosymra) and diazepam (Valtoco) and has been shown to increase the absorption of nalmefene.1
Figure 2 lists some other permeability enhancers investigated during clinical trials. Surfactants can enhance absorption with more than one mechanism – these include perturbing the cell membrane by leaching of membrane proteins, opening of tight junctions or preventing enzymatic degradation of the drugs. These surfactants are mainly used and studied in oral drug administration. However, there have been several studies looking at their application in nasal and pulmonary drug delivery.
| SELECTED PERMEABILITY ENHANCERS & SOLUBILISERS |
| • Intravail • Polysorbate 20/80 • Cyclodextrins • Lecithin • HPMC • Oleic Acid • Propylene Glycol |
Figure 2: Permeability enhancers.
Surfactants such as polysorbates and lecithin, for example, have been found to increase the solubility of both the active and its permeability.
Modifying the inhaled particle surface with agents that enhance their absorption is a potential route to formulation strategy. For example, spray-dried, polymer-coated liposomes composed of soy phosphatidylcholine and phospholipid dimyristoyl phosphatidylglycerol coated with alginate, chitosan or trimethyl chitosan increased penetration of liposomes through the nasal mucosa over uncoated liposomes when delivered as a dry powder.
OPTIMISING SYSTEMIC ABSORPTION THROUGH DEVICE SELECTION
A key requirement of the delivery device is the compatibility with the formulated product with regard to stability. It is important to establish if there is any observation of degradation of the product that is being influenced by the materials of construction. The design must be user friendly and be reliable in use to give consistent metering across the life of the product for multi-dose devices. All materials of construction should be reviewed and an assessment of potential extractables/leachables and adsorptive properties should be made. Various orifice and actuator combinations are available, so better targeted delivery can be achieved through careful selection.
There are a multitude of devices to select from, including the traditional multidose aqueous spray pumps – which deposit the drug primarily at the front of the nose, not reaching much further – and monodose sprays which have a similar performance. But there are several other types of device to consider that can lead to greater deposition towards the back of the nasal cavity, such as dry-powder devices, which can drive the drug deeper into the nasal cavity (e.g. Optinose’s Exhalation Delivery Systems, and Aptar Pharma’s UDS). There are also nasal pMDIs, which use a volatile propellant so are less likely to drip out of the nose, and nebulisers that create small droplets that can be inhaled further into the nose. Nemera is currently developing a pMDI device (RetroNose) that is actuated into the mouth and then exhaled through the back of the nasal cavity, giving a greater deposition in the areas of interest.
By combining the formulation development with device selection, it is possible to maximise the systemic exposure of the therapeutic by a combination of targeted delivery to the areas of the nasal cavity giving optimal absorption characteristics, reducing the clearance time from these areas and accelerating the absorption while resident. When making this selection, it is important to consider the therapeutic use and dosing regimen (whether multidose daily treatment or monodose for vaccine or rescue medicines), drug cost, device costs, potential intellectual property, drug/excipient interactions, device interactions (whether small molecule or biologic), patient demographic and ease of use.
INTERTEK SOLUTIONS
The recent expansion at our Centre of Excellence for Inhaled and Nasal Drug Development in Melbourn, UK, has focused on new, powerful in vitro analytical strategies, integrated with formulation, stability and clinical trial material manufacturing to enable our clients’ key decision-making activities throughout the product development lifecycle.
The Intertek formulation development team offers design and optimisation of formulations for nasal drug products as well as powders, capsules, liquids and solids, semi-solids, inhaled, nebulised, pressurised and topical drug formulations. We provide focused understanding from an early stage of development tailored to your new chemical entities and generic products, from feasibility through to development support, Phase I and II clinical trials, scale-up and transfer to commercial manufacturing.
Our expertise helps accelerate project timelines and includes preformulation, excipient-API compatibility assessment and optimisation, physicochemical testing, formulation screening, lab-scale formulation and accelerated stability studies to achieve the desired product characteristics. Prior to preclinical studies, we can offer a range of analytical capabilities including solubility assessment, dissolution, solid state characterisation, particle morphology (Malvern Morphologi 4 ID), forced degradation and stability screening, in order to select the optimal development candidates.
Our experience in powder characterisation can drive insight into understanding powder-formulation characteristics, and our physical and chemical testing methods can determine particle size (light scattering, microscopy), thermal properties (DSC, TGA), powder rheology, morphology (powder X-ray diffraction) and spectroscopic profiles (FTIR, Raman).
The approach taken by the Intertek formulation development team enables small quantities of drug product to be developed using experimental design methodologies supported by testing at every stage. By integrating screening, analysis and stability storage, our specialists can provide a range of formulations in a timely and cost-effective manner in order to identify the most promising candidates to progress through to clinical development. As a result, we can save you time by reducing method and technology transfer time as well as effort.
With a holistic approach to service provision – including raw material quality control, scale-up, pilot-scale batch manufacturing and testing, GMP clinical batch manufacturing, stability storage and impurities testing, as well as release testing with qualified person release – we offer a one-source solution for material supplies for use in Phase I and II clinical trials.
REFERENCES
- Philip Krieter P, Gyaw S, Crystal R, Skolnick P, “Fighting fire with fire: development of intranasal nalmefene to treat synthetic opioid overdose”. J Pharmacol Exp Ther, 2019, Vol 371(2), pp 409–415.

