To Issue 174
Citation: Pidgeon A, “Smart Enough: Designing Drug Delivery Devices that Put Patients First”. ONdrugDelivery, Issue 174 (Jun 2025), pp 12–15.
Andy Pidgeon challenges the assumption that more advanced technology is always better, re-examining the design approach to connected autoinjectors from the patient perspective and highlighting the value of simplicity and usability – digging into the idea that, by investigating the real-world needs of patients, drug delivery device designers can ensure that their devices are serving those needs, rather than creating unnecessary new challenges for users.
“THE AIM IS TO SHIFT FOCUS BACK TO SIMPLICITY, RELIABILITY AND USABILITY, SUPPORTED BY REAL-WORLD EVIDENCE.”
INNOVATING FOR PATIENTS, NOT TECHNOLOGY
As a designer of drug delivery devices, and a passionate advocate for patient usability, I have learned that innovation only matters if it truly helps real patients. In the rush to create “smart” connected autoinjectors, the drug delivery industry risks forgetting that many patients just want something simple, reliable and easy to use. The real question is not how advanced we can make our devices, but whether or not those features are solving critical user needs.
This article explores how development teams can choose technologies that genuinely support patients, rather than adding features merely for the sake of progress. From artificial intelligence (AI) and Bluetooth to wearable injectors and platform designs, it will look at where technology adds value and where it adds unnecessary complexity. It will also examine the challenges of delivering high-viscosity, high-volume drugs and question whether features such as skin sensors benefit patients or simply reassure manufacturers. The aim is to shift focus back to simplicity, reliability and usability, supported by real-world evidence.
“IT MUST BE ASKED: ARE THESE FEATURES GENUINELY HELPING PATIENTS, OR JUST TICKING THE INNOVATION BOX?”
THE ALLURE OF “SMART” INJECTORS VERSUS PATIENT REALITIES
It is tempting to imagine a fully connected autoinjector ecosystem – syncing to an app, logging each dose, providing feedback and perhaps even offering AI-powered coaching. In theory, this promises better adherence, useful data for clinicians and more empowered patients. But it must be asked: are these features genuinely helping patients, or just ticking the innovation box?
Too often, high-tech devices are launched without clear evidence they meet a real patient need. Non-adherence is a genuine issue, and connected devices are often seen as the answer, with some studies showing encouraging adherence1 – one showed over 90% adherence in multiple sclerosis patients using a connected injector and app over a year.2 However, the number of patients using the device dropped to 76% after one year, so many of these positive studies are short-term and may not reflect long-term behaviour.
On the ground, complexity can make things worse. I have seen patients with arthritis struggle with tiny Bluetooth buttons, and others sigh in frustration at pairing requirements. Simplicity should not be seen as a compromise – it is often the best design choice.
As designers, we also need to ask who we are designing for. A tech-savvy early adopter may welcome new features, but many patients are older, time-poor or anxious, and just want treatment that works without fuss. If technology makes their lives harder, it has failed, no matter how advanced it looks (Figure 1).
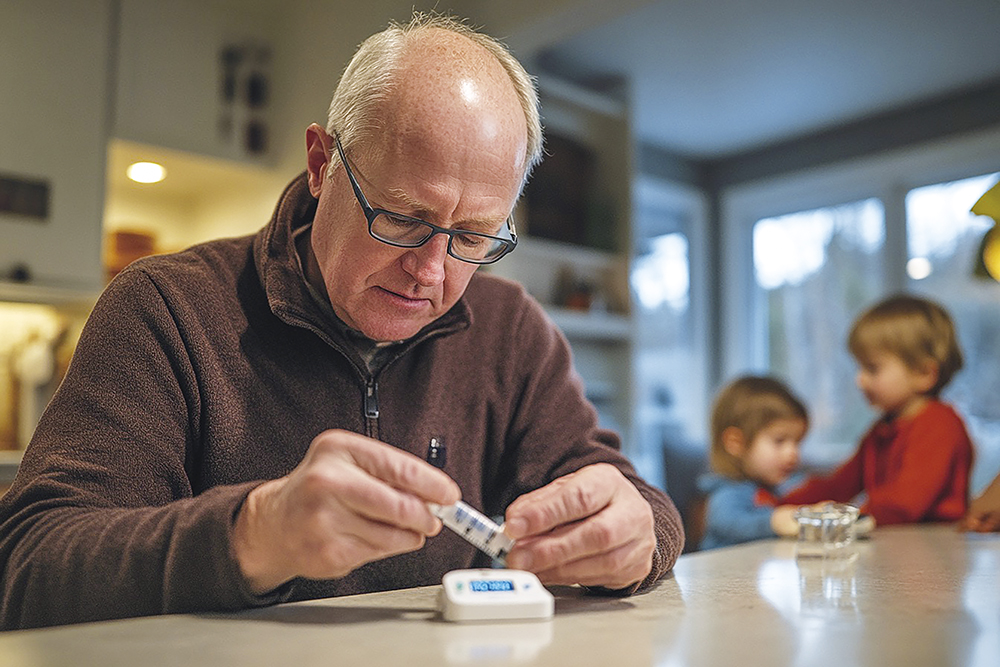
Figure 1: It is crucial to keep the intended user, along with their specific desires and problems, in mind throughout the design process.
Adherence is not always about forgetfulness. Most self-injecting patients do not forget their dose – it is often uncomfortable and emotionally charged. Many patients build routines around it. Others choose to skip a dose to feel in control – a small act of agency in a life shaped by treatment. No flashing LED or push notification will change that.
WHEN COMPLEXITY CREEPS IN – THE PITFALLS OF HIGH-TECH FEATURES
Looking under the bonnet of today’s smart injectors, a few recurring “features” stand out – both their potential and their pitfalls.
Bluetooth Connectivity (and the Pairing Problem)
Most connected devices use Bluetooth to sync data to an app. In theory, this works in the background. In practice, pairing can be difficult, especially when users are already anxious. Entering codes or changing phone settings adds pressure. Some devices now avoid this with automatic Bluetooth or near-field communication (NFC), which does not require pairing.3 This seamless approach matters, as even scanning a QR code each time a patient needs to inject can become an unwanted chore. Unless a feature works instantly and effortlessly during use, patients will avoid it – and frustration can outweigh any potential benefit.
AI-Driven Guidance and Reminders
AI is becoming a common feature in healthcare, including drug delivery. It is often imagined as a helpful digital nurse – reminding patients when to inject, offering tips and, perhaps one day, adjusting doses. This vision is appealing, especially if AI can learn habits and provide support in the background.
However, designers must be cautious. If AI starts giving instructions without explanation – such as telling a patient to delay a dose – it may lead to confusion or conflict with clinical advice. Patients and clinicians need to understand and trust what AI is doing, and it must be clear who is accountable if it gets things wrong. The danger of black box decisions is very real.
To be genuinely useful, AI features must be transparent, easy to understand and optional. For now, its best use may be supporting adherence behind the scenes. Because no matter how advanced the technology, the key to successful treatment is still a person who feels confident using it.
WEARABLES AND HIGH-VOLUME DELIVERY
A key challenge in injector design is the rise of biologic drugs needing larger volumes or higher viscosities. Standard spring-loaded pens can manage around 1 mL without trouble, but pushing more than 2 mL of a thick antibody solution through a fine needle is another story – the forces required skyrocket as viscosity increases.4
This is where wearable injectors come in. Worn like a patch, these devices deliver medication slowly over time, making large doses more comfortable. These devices are ideal when volumes exceed 2–3 mL, a limit for most autoinjectors. Though bulkier, their real value lies in solving a real need – reliable home delivery of difficult drugs.
While some wearable injectors include connectivity to track doses, their main strength is mechanical – not digital. They reduce patient burden and improve access without unnecessary complexity. Rather than adding smart features for their own sake, we should take cues from these devices: identify real barriers to treatment and use technology to remove them.
OFF-THE-SHELF PLATFORMS VERSUS BESPOKE SOLUTIONS
Autoinjectors were once bespoke for each drug. Now, platform devices offer pre-designed solutions that pharma teams can adapt. These platforms have already been tested with different volumes and syringe types, saving time and cost while improving reliability. Owen Mumford’s (Woodstock, UK) Aidaptus, for example, claims to fit both 1 mL and 2.25 mL syringes, automatically adjusting to varying fill volumes.5 This flexibility is especially useful during clinical trials or if doses change. Platforms such as Aidaptus also offer smart features, but only where needed. The core device is simple, robust and designed for ease of use. Optional extras like NFC and sensors can be added later.
“A MODULAR APPROACH KEEPS THE FOCUS ON USABILITY WHILE AVOIDING OVER-ENGINEERING. INSTEAD OF BUILDING COMPLEX SYSTEMS FROM THE GROUND UP, PLATFORMS ALLOW DEVELOPERS TO CHOOSE THE FEATURES THAT BENEFIT PATIENTS.”
A modular approach keeps the focus on usability while avoiding over-engineering. Instead of building complex systems from the ground up, platforms allow developers to choose the features that benefit patients. It is a more efficient, patient-centric way to innovate – one where technology earns its place rather than being included by default.
SKIN SENSORS AND SAFETY INTERLOCKS
A subtler example of potential over-engineering is the use of skin contact sensors in some electromechanical injectors. These aim to prevent misfires unless the device is correctly positioned, and to stop the injection if it is pulled away mid-dose. While this sounds helpful, the real-world need is debatable.
Traditional spring-loaded injectors managed safety with mechanical features alone – the patient had to press firmly to trigger the spring, and the dose was delivered in seconds, limiting the chance of early removal. Electronic injectors often take longer, with start and pause buttons and variable speeds, so designers introduced sensors to pause and retract if contact is lost.
For instance, UCB’s (Brussels, Belgium) ava Connect can halt injection and resume after repositioning, preventing wasted doses.6 This is clever, but is the added complexity really essential? A clear “do not remove” indicator and proper training may be enough in most cases. Skin sensors can be useful, but they add cost, use power and may fail. Of course, this approach is helpful for gaining adherence data, but is it useful for the patient? Unless a therapy frequently faces interrupted injections, such features may be better used selectively, not by default.
CHOOSING TECH THAT EARNS ITS PLACE
How, then, do designers decide which innovations to include and which to leave on the cutting-room floor? The following are a few guiding principles can help keep us honest.
Always Start with the User Problem
Before adding any feature, be clear about which patient problem it addresses. Is forgetfulness the issue? A simple SMS reminder might be enough. Is needle anxiety causing hesitation? A hidden needle or slower injection could help. Every added feature should answer the question: “What specific user pain point does this solve, and have we verified that the problem really exists?”. If the benefit is unclear, or a simpler solution exists, reconsider. Before adding another app, chip or update, always ask: “What real problem are we solving?”
Complexity Must Earn Its Place
This oft-repeated design principle means any added complexity – mechanical, electrical or digital – must bring clear, proportionate benefit. It is tempting to include features because they might be useful in some cases but, if only a few gain from them while all users have to deal with the added burden, they do not justify inclusion. For example, streaming detailed injection force data to the cloud might appeal to the engineering team, but it rarely improves patient care. Beyond confirming a dose was taken, extra data “provides no additional added value”3 and can even clutter the system. Designers should be ruthless in pruning features that are cool in theory but superfluous in reality.
“REAL-WORLD STUDIES REVEAL ISSUES LIKE PATIENTS FORGETTING TO SYNC BLUETOOTH OR SKIPPING INJECTION AIDS THAT SLOW THEM DOWN, EVEN IF IT ONLY ADDS A MINUTE TO
THEIR ROUTINE.”
Design for the Worst-Case User, Not the Ideal User
To truly make devices inclusive, imagine the person least likely to succeed with a device, and make it work for them. That might be someone who has never used a smartphone, has limited dexterity or is too busy to read the manual. Real-world studies reveal issues like patients forgetting to sync Bluetooth or skipping injection aids that slow them down, even if it only adds a minute to their routine.
These insights can help to simplify the design. Perhaps the device always stays on in a low power mode, removing the need for a power switch. Maybe it comes pre-paired to avoid setup. Or maybe it includes a mechanical backup, like the Owen Mumford UniSafe, to ensure that the injection works even if the electronics fail.7 Empathy in design should lead to real, practical decisions that make the device easier for everyone to use.
Embrace Simplicity as an Outcome
It is easy to think that “simple” means “unsophisticated,” but designing something that feels simple takes real skill. The best autoinjectors are often one-step devices – remove the cap, press to the skin and the injection is done. They appear straightforward, yet involve precise engineering for needle control, drug delivery and safety. We should celebrate designs that achieve more with less – using clever mechanical ideas rather than relying on electronics.
Focusing on the essentials often creates more reliable, user-friendly devices. Even companies building advanced injectors prioritise clear, patient-focused design. Technology should support care, not get in the way. Sometimes the smartest approach is to reduce features and focus on what matters most – ease, clarity and confidence.
Provide Value to All Stakeholders – But Prioritise the Patient
This is a delicate balance – healthcare providers and pharma companies value the data from connected devices, but, if collecting it worsens the patient experience, it becomes counterproductive. The user experience must come first, even if that means gathering less data.
There is a tendency to want to satisfy everyone – doctors ask for adherence logs (though most do not use them), marketing wants a flashy app and regulators want layers of safety. The result is often an overbuilt device that suits no one, especially not the patient. A better solution is offering a range of device options. Simplicity for those who want it, technology for those who need it. This kind of choice respects individual needs and helps developers stay grounded – if most people avoid the tech heavy option, it may be time to reassess what really adds value.
REDEFINING “INNOVATION” IN DRUG DELIVERY
True innovation in pharmaceutical devices is not about cramming the most technology possible into a product; it is about intelligently applying technology to solve meaningful problems. A connected injector is only useful if it improves outcomes without adding effort. A wearable injector that enables at-home treatment is valuable because it improves quality of life. Features that confuse or overwhelm users are not progress.
Designers should shift from asking “What can we add?” to “What should we add to make things better for patients?” Sometimes that means advanced technology, and sometimes it means a simpler shape or clearer instructions. Perhaps the most patient-centric innovation is simply a better ergonomic shape that an elderly patient can hold securely in their hand, or a Bluetooth implementation that does not require pairing or user thought – it just works out of the box. Every new feature should be judged on whether it improves simplicity, usability, reliability or empathy. If it does not, it may not belong.
FINAL THOUGHTS
The future of drug delivery will bring more digital and connected tools, and that can be a good thing – if used wisely. Success should be measured by whether patients can and will use the device with confidence. Impressive features mean little if they complicate the experience or stop treatment from happening.
We must design for people, not platforms, and recognise when a simpler approach is actually more effective. Real-world feedback should guide us, not just what works in the lab. True innovation lies in knowing what to add – and what to leave out. Simplicity, used well, is powerful.
REFERENCES
- Antalfy A et al, “The Adherence and Outcomes Benefits of Using a Connected, Reusable Auto-Injector for Self-Injecting Biologics: A Narrative Review”. Adv Ther, 2023, Vol 40(11), pp 4758–4776.
- Bryson S, “Most Patients Adhere to Betaseron Therapy Over 1 Year, App Data Show”. Multiple Sclerosis News Today, Mar 2022.
- Song J, “Key Design Considerations For Digitally Connected Injectors”. Med Device Online, May 2022.
- Roe MJ, “Challenges in High- Viscosity, High-Volume Drug Delivery”. ONdrugDelivery, Issue 125 (Oct 2021), pp 40–43.
- “Aidaptus – The next generation platform disposable auto-injector”. Manufacturing Chemist, Mar 2022.
- “UCB Gains CE Mark for ava Connect®, a first-in-class electromechanical device for use with biologic treatment in rheumatology and dermatology”. Press Release, UCB, Mar 2021.
- “UniSafe® 1mL Auto-injector”. Company Web Page, Owen Mumford, Accessed May 2025.


